BY: ELISABETH WRIGHT BURAK, MPP, MSW
Illustration by: Nancy Stahl
Medicaid provides health coverage to the nation's lowest income and most vulnerable children. Many of these children have higher health care needs than the general population and live in families without the resources to pay for needed care. Medicaid's comprehensive, child-focused benefits are uniquely designed to meet these higher health care needs and to maximize a child's potential by addressing developmental delays and health conditions that affect school performance and success in life.1
Continuous, consistent health care coverage without disruptions is especially critical for young children. A child's brain develops most rapidly in the earliest years of life, building the foundation for learning, behavior and health. Health care coverage is one of the critical first steps toward ensuring children get what they need to pave the way for school readiness and overall physical, social and emotional health impacting them well into adulthood.
Experts recommend 16 well-child visits before age 6.2 Medicaid makes such crucial care available for more than one-third of America's children.3 These visits allow pediatricians and family practitioners to closely monitor a child's development and address any concerns or delays as early as possible. Well-child visits also hold potential for medical providers to screen and address the broader social, economic, educational, environmental and related needs of the children and their families.
Children make up the single largest group of individuals who rely on Medicaid for their health care coverage.4 Medicaid helps children get healthy and stay healthy so they are ready to learn in the classroom.5 Research shows that health coverage can reduce school absenteeism by increasing children's checkups and overall health.6 We also know from longitudinal research that Medicaid leads to children's education and economic success in adulthood, even making the difference in whether or not a child graduates from high school or college.7 Childhood Medicaid coverage produces economic benefits in adulthood, including increased employment, higher tax payments and returns on public investment in Medicaid.8 Researchers also have found that Medicaid coverage during childhood leads to better overall health during adulthood.9
A CHILD-CENTERED BENEFIT PACKAGE
One of the most important features of Medicaid is its child-centered benefit package, known as Early Periodic Screening Diagnostic and Treatment (EPSDT). Ensuring more comprehensive and preventive coverage compared to private plans or even Medicaid benefits for adults, EPSDT is the definitive standard for children's health coverage. Its aim is to make sure that children receive all the pediatrician-recommended preventive screenings and health care services they need to stay on track developmentally. This important provision helps give our nation's most vulnerable children the best shot at reaching their full potential. And states can do more to ensure the promise of EPSDT is fully realized, by improving data collection and transparency, implementing a comprehensive child health quality focus, or prioritizing and integrating pediatric care in state payment and delivery system reform efforts. This helps states gain a better understanding of whether children get the care they need when they need it and where areas for improvement exist.10
One area for possible focus is whether all children receive preventive screenings, such as developmental screenings, and any necessary follow-up services that emerge. As highlighted in a Center for Children and Families brief on developmental screenings and the Children's Health Insurance Program from earlier this year: "Routine screening for all children is an important gateway to ensure those identified with certain delays or needs receive early intervention or other appropriate services that can help them meet developmental milestones and enter school ready to learn."11
As many as 1 in 4 children under age 6 may be at moderate or high risk for developmental, behavioral or social delays.12 Larger shares of young children of color are at risk for delays compared with their white peers. Young children living in poverty (100 percent of the federal poverty line) are more than twice as likely to be at high risk of developmental delay than those in families with incomes more than double the poverty line (above 200 percent of the federal poverty line).13
COVERING PARENTS HELPS CHILDREN, TOO
Medicaid coverage also helps children by covering some of the adults in their lives, such as parents or caregivers, even before they are born. That's because the health of parents, caregivers and other adults in a child's life has a direct influence on the child's healthy development.14 When pregnant women have access to Medicaid, newborns in low-income families have a better chance at a healthy birth and a strong start during their critical first year of life.
Young children's brain development relies on positive, nurturing interactions with parents and caregivers.15 A growing number of states are exploring new ways to support parents as key actors in their children's healthy development. For example, an increasing number of states — now 32 — cover maternal depression screenings as part of a child's Medicaid well-child visits, providing another line of intervention to help parents connect to needed mental health treatment.16 Screening mothers for depression as part of a child's well visit, and then taking steps to refer them to follow-up treatment, recognizes the close link between maternal well-being and healthy child development. Moms experiencing depression have a harder time bonding with and caring for their children. A report from the American Academy of Pediatrics found that children living with mothers with depression may "…show impaired social interactions and delays in development."17 Mothers from lower income brackets are more likely to experience depression than moms with higher incomes. Between 40 and 60 percent of low-income women report experiencing some depressive symptoms, compared with 5 percent to 25 percent of all pregnant, postpartum and parenting women, the AAP report found.18
Medicaid coverage for parents also improves children's access to health care and their overall well-being. When parents are insured, their children are almost guaranteed to be covered, too. A study found evidence of the "welcome mat" effect in states that expanded Medicaid to adults, estimating that over 700,000 children who were already eligible for Medicaid were enrolled between 2013 and 2015. This means that as parents gained coverage, their children—most already eligible for Medicaid but not enrolled—got signed up, too. The benefits of Medicaid expansion to parents extends beyond coverage itself. A Pediatrics study found that Medicaid eligibility expansions for parents between 2001 and 2013 were associated with an increased probability of low-income children having a well-child visit.19
Parent health itself also impacts children. When parents get the care they need to get and stay healthy, it can improve their ability to support their children's learning and engage more in school activities. Health coverage for the whole family eases the financial stress of a medical emergency or accident. Medicaid effectively shields many children from poverty while providing peace of mind for parents.
PROGRESS COVERING CHILDREN AT RISK
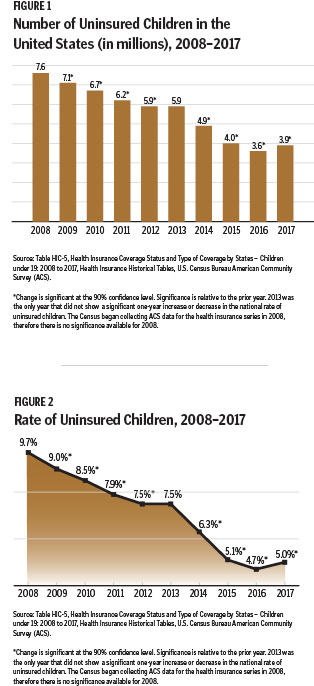
Medicaid's role for children cannot be overstated. Working together with CHIP, Medicaid has played a major role in driving down the uninsured rate for children to a historic level of 4.7 percent in 2016.
However, for the first time in nearly a decade, the nation's steady progress in reducing the number of uninsured children actually reversed course last year. Data from the U.S. Census Bureau shows the number of uninsured children under age 19 nationwide increased by 276,000 to just over 3.9 million in 2017 (Figure 1).20 The rate of uninsured children ticked upward from the historic low of 4.7 percent to 5 percent (Figure 2).
There is no single reason for the coverage loss for children, but there are many factors that likely contributed. The lengthy and ultimately unsuccessful congressional effort to repeal the Affordable Care Act and cap federal Medicaid funding, along with the unprecedented delay in Congressional action that allowed the CHIP funding to temporarily lapse, likely played a role by sending the message that publicly funded coverage was at risk. In addition, Congress repealed the ACA's individual mandate, and the Trump administration made numerous efforts to undermine the ACA insurance marketplaces, including dramatic cuts in outreach and enrollment grants and a shortening of the open enrollment period.
Another contributing factor could be the changes in state Medicaid information technology systems that may have added red tape for families applying for or renewing coverage. Finally, given that one quarter of all children in the U.S. have a parent who is an immigrant, the policies and rhetoric targeting immigrant communities likely deterred parents from enrolling their eligible children in Medicaid or CHIP, despite the fact that most of these children are U.S. citizens.
This increase in the uninsured rate for children should serve as an important warning sign to policymakers. Uninsured children are more likely to have unmet health needs and lack a usual source of care.21 Untreated medical conditions such as asthma lead to missed school days and reduce children's chances for success in school.22 This national trend raises concern about whether or not all children will have the opportunity to grow and thrive. Barring any serious efforts to get back on track, there is every reason to believe the decline in coverage for children is likely to continue and possibly get worse.
ELISABETH WRIGHT BURAK is a senior fellow at Georgetown University McCourt School of Public Policy's Center for Children and Families.
NOTES
This article is based on research available on the Georgetown University Center for Children and Families website ccf.georgetown.edu and other sources as noted below.
- Joan Alker and Alisa Chester, "Children's Health Coverage Rate Now at Historic High of 95 Percent," Georgetown University Center for Children and Families, October 2016. See also Data Resource Center for Child & Adolescent Health, National Survey of Children's Health "What type of health insurance coverage, if any, did [child name] have at the time of the survey? 2011/12. And Rob Geen, Anna S. Sommers and Mindy Cohen, "Medicaid Spending on Foster Children," The Urban Institute, August 2005, www.urban.org/research/publication/medicaid-spending-foster-children.
- Committee on Practice and Ambulatory Medicine, Bright Futures Periodicity Schedule Workgroup, "Recommendations for Preventive Pediatric Health Care," American Academy of Pediatrics, 2017, http://pediatrics.aappublications.org/content/139/4/e20170254.
- Joan Alker and Olivia Pham, "Nation's Progress on Children's Health Coverage Reverses Course," Georgetown University Center for Children and Families, November 2018, https://ccf.georgetown.edu/2018/11/21/nations-progress-on-childrens-health-coverage-reverses-course/.
- "2016 Actuarial Report on the Financial Outlook for Medicaid," Office of the Actuary, Centers for Medicare and Medicaid Services, 2016.
- Karina Wagnerman, Alisa Chester and Joan Alker, "Medicaid Is a Smart Investment in Children," Georgetown University Center for Children and Families, March 2017.
- Shishu Zhang, "Do Our Children Become Healthier and Wiser? A Study of the Effect of Medicaid Coverage on School Absenteeism," International Journal of Health Services 42, no. 4 (2012): 627-46.
- Wagnerman, Chester and Alker, "Medicaid Is a Smart Investment."
- Wagnerman, Chester and Alker, "Medicaid Is a Smart Investment."
- Wagnerman, Chester and Alker, "Medicaid Is a Smart Investment."
- For these and other recommendations, see Elisabeth Wright Burak, "Promoting Young Children's Healthy Development in Medicaid and CHIP," Georgetown University Center for Children and Families, October 2018, https://ccf.georgetown.edu/2018/10/17/promoting-young-childrens-healthy-development-in-medicaid-and-the-childrens-health-insurance-program-chip/; Andy Schneider and Stephanie Altman, archived webinar, "How Can We Tell Whether Medicaid MCOs Are Doing a Good Job for Kids?" Georgetown University Center for Children and Families, February 14, 2018, https://ccf.georgetown.edu/2018/02/14/live-webinar-how-can-we-tell-whether-medicaid-mcos-are-doing-a-good-job-for-kids/.
- Elisabeth Burak and Mike Odeh, "Developmental Screenings for Young Children in Medicaid and the Children's Health Insurance Program," Georgetown University Center for Children and Families, March 2018, https://ccf.georgetown.edu/2018/03/06/developmental-screenings-for-young-children-in-medicaid-and-the-childrens-health-insurance-program/.
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, The Health and Well-Being of Children: A Portrait of States and the Nation, 2011-2012. " (Rockville, Maryland: U.S. Health and Human Services, 2014).
- HHS, The Health and Well-Being of Children.
- Burak, "Promoting Young Children's Healthy Development."
- "From Best Practices to Breakthrough Impacts: A Science-Based Approach to Building a More Promising Future for Young Children and Families," Center on the Developing Child at Harvard University, (2016), https://developingchild.harvard.edu/resources/from-best-practices-to-breakthrough-impacts/.
- Sheila Smith et al. "How States Use Medicaid to Cover Key Infant and Early Childhood Mental Health Services: 2018 Update of a 50-State Survey, " National Center for Children in Poverty, November 2018.
- Marian F. Earls and the Committee on Psychosocial Aspects of Child and Family Health, "Clinical Report—Incorporating Recognition and Management of Perinatal and Postpartum Depression Into Pediatric Practice," Pediatrics, 126, no. 5 (2010): 1032-39.
- Earls et al., "Clinical Report."
- Maya Venkataramani, Craig Evan Pollack and Eric T. Roberts, "Spillover Effects of Adult Medicaid Expansions on Children's Use of Preventive Services," Pediatrics 140, no. 6 (2017).
- Alker and Pham, "Nation's Progress on Children's Health Coverage."
- Robin Rudowitz, Samantha Artiga and Rachel Arguello, "Children's Health Coverage: Medicaid, CHIP and the ACA," Kaiser Family Foundation, March 2014.
- "Asthma-Related Missed School Days among Children aged 5–17 Years," Centers for Disease Control and Prevention, October 2015, www.cdc.gov/asthma/asthma_stats/missing_days.htm; "The Relationship Between School Attendance and Health," Robert Wood Johnson Foundation, September 2016, https://www.rwjf.org/en/library/research/2016/09/the-relationship-between-school-attendance-and-health.html.