BY: REV. MICHELE J. GUEST LOWERY, MDiv, BCC
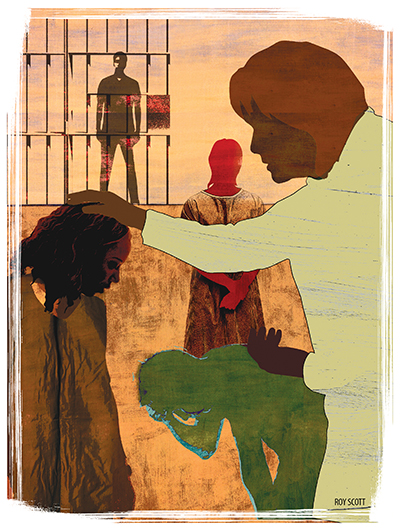
Illustration by: Roy Scott
You receive a call to the emergency room: A patient admitted for observation has requested spiritual support. When you arrive, the patient greets you with a torrent of words, rapidly shifting from topic to topic. She becomes agitated when you try to respond. You are not sure what to do.
A patient in the spirituality group you facilitate is convinced he has committed the unpardonable sin. He relentlessly seeks reassurance from you and others, yet his fear not only persists but intensifies. You are at your wit's end.
You receive a call from a local pastor. One of his parishioners has a chronic mental disorder and is becoming disruptive during services. Members of the church are torn between their desire to offer compassionate support and their growing frustration with — and fear of — the person's behaviors. What counsel do you offer this colleague in ministry?
There are arguably few areas in ministry more challenging to even seasoned chaplains than behavioral health. The reason is straightforward: Opportunities for chaplaincy training in this area are limited largely to the occasional general hospital psychiatric unit rotation or didactic in clinical pastoral education programs. Yet chaplains encounter people with mental illness every day — in the emergency room, awaiting surgery, visiting a hospitalized family member, in prison, at a nursing home. How can we best serve those living with mental disorders?
UNDERSTANDING BEHAVIORAL HEALTH
Behavioral health refers to the field of mental health care comprising both mental illness and addiction. It embraces a recovery model that includes treatment of the whole person, not just illness symptoms. By focusing on behaviors that promote stabilization and wellness, this treatment approach helps patients learn skills and strategies for effective living.
Mental illness is a collective term for a group of disorders affecting how a person thinks, feels and behaves, thus compromising all aspects of daily functioning. These disorders are classified according to representative symptoms. For example, psychotic disorders are characterized by loss of touch with reality. Hallmark symptoms include hallucinations — sensations that seem real but are created in one's mind — and delusions — strongly held, false beliefs not consistent with one's culture. Schizophrenia is the most common psychotic disorder.
Mood disorders are another major category of mental illness, characterized by significant disturbance in one's emotional state. Depressive disorders are marked by persistent sadness or loss of interest in previously enjoyed activities. Bipolar disorder causes dramatic shifts in mood, from depressive "lows" to periods of abnormally high energy and euphoria, called manic episodes.
There is no exact science on why a person develops a particular mental disorder. However, research strongly suggests that most mental disorders are caused by the interplay between heredity, brain biochemistry and environmental factors. This is why mental illness is called a brain disease. Useful resources for learning about the various mental disorders include the Statistical Manual of Mental Disorders, now in its fifth edition (DSM-V); the National Institute of Mental Health (nimh.nih.gov); the National Alliance on Mental Illness (nami.org); and the American Foundation for Suicide Prevention (afsp.org)
THE IMPACT OF STIGMA
Although we have come a long way in our understanding of mental illness, misconceptions persist, fueled by fear, outdated belief systems, media sensationalism and misinterpretation of sacred texts. Some still attribute mental illness to personal weakness. Others see it as a spiritual issue: lack of faith, sin or demonic possession. In the aftermath of mass shootings and other public acts of violence, mental illness consistently is scapegoated.
"Jack" is admitted to the psychiatric hospital where I work. He refuses to take medication. He refuses to participate in any form of treatment or recreational activity. Day after day, he sits alone in his room, praying for a miracle.
Jack's father, devoutly religious, will not accept that his only son has schizophrenia. He fervently believes that with faith and prayer, his son will be healed. Jack doesn't want to disappoint his father. He feels shame that he hasn't been healed.
The impact of stigma is complex and deeply debilitating. Its consequences include discrimination, social isolation and a sense of self as irreparably flawed. When fused with one's spiritual beliefs, it can result in self-punishing behaviors as "atonement" for perceived sins, treatment resistance and chronic seeking of religious miracles. Although there are no "quick fixes" or easy answers for confronting stigma, the following guidelines are fundamental:
Don't label people. Ever. People with mental disorders are not "crazy," "loony," "basket cases" or "frequent fliers." This kind of labeling is blatantly disrespectful and perpetuates stereotyping. Labeling people by their diagnosis is also inappropriate. Instead of calling someone "a schizophrenic," identify someone with a specific mental disorder as "a person with schizophrenia" or "an individual who has bipolar disorder." This is called person-first language, reminding us that illness is an experience in life, not one's identity as a person.
Consistently reinforce the message "you are not your illness." The most damaging aspect of stigma is arguably over-identification with one's mental disorder, thus seeing one's self as less than whole. By helping people embrace the larger context of their lives, we remind them that they are valued, capable and worthy of love. We remind them that they, too, are created in the image of the Divine.
Never underestimate the power of presence in healing. A formative book in my life is The Little Prince by Antoine de Saint Exupery, chock-full of timeless truths. I especially love the vignette in which a fox teaches the prince how to, step by step, establish meaningful ties: Be patient, sit quietly, approach slowly, keep showing up at the appointed time. I decide to try this approach with "Jack."
I introduce myself to Jack and ask if I can just sit with him. He scowls and growls: "I don't want any lectures or sermons."
"Got it," I reply, and sit quietly across the room for 15 minutes. As I get up to leave, I ask permission to return the following day.
"If you want to waste your time," he replies.
Day after day, I come back at the same time, sitting quietly, no words exchanged. Then one day he speaks: "Don't you worry what people think about you hanging out with a bad, crazy schizophrenic?"
"No," I reply, "because I don't believe you're either bad or crazy. You just have a mental illness. People get sick, Jack. Some have diabetes, some have heart disease, some have mental disorders."
He returns to his characteristic silence, but as I leave, he says: "My dad has heart disease."
When I return the next day he is pacing.
"Tell me one thing," he says. "If I'm not bad, then why doesn't God answer my prayers for a miracle?"
I don't answer right away. Finally, I say, "Maybe he already has. Maybe the miracle is medication that can help you. Maybe it's learning you're bigger than your illness. Maybe the miracle is a lot of things other than a cure."
Jack looks thunderstruck and says, "My father takes medicine for his heart. If he didn't, he would die."
The next day, Jack comes out of his room. Tentatively, haltingly but surely, he engages in treatment and begins to believe he can recover.
BOUNDARY CONSIDERATIONS
There's a twofold dimension to boundary considerations in behavioral health: meticulous maintenance of our own boundaries and management of intrusive, chaotic and/or aggressive patient behaviors.
Mental disorders have a significant impact on a person's perceptions, sensory processing and emotional regulation. Touch, for example, can trigger flashbacks in trauma survivors, evoke unwanted memories and provoke strong reactions. It also can be physically painful to people with tactile hypersensitivity, common to some disorders. Simple gestures of caring — a squeeze of the hand, hug or pat on the back — may be interpreted as intimate acts. For these reasons, touch of any kind is highly discouraged, if not prohibited, in behavioral health settings.
Other professional boundary issues include self-disclosure and patient interactions that could be perceived as "special treatment." Patients with active mental disorders can be highly suggestible, vulnerable to influence and deeply lonely. They may distract from their treatment by caretaking you if you disclose personal information. They may mimic your expressed opinions and beliefs. They may infer a special relationship from special consideration. Carefully reflect on whose needs are being served with every interaction and intervention. Crossing boundaries, no matter how well intended, can cause harm.
Managing disruptive patient behaviors is an aspect of boundaries that can be especially challenging for chaplains, who often aren't trained in behavioral management strategies and may feel intimidated or fearful. We need to learn how we can respectfully redirect patients who become intrusive or aggressive, while keeping others and ourselves safe.
Remember: It's not about you. Different mental disorders alter a person's behavior in distinct ways. That hyper-verbal patient who suddenly becomes irritable toward you likely is experiencing mania. The group member who begins gesturing and talking loudly without provocation may be hearing voices. The patient who fixates on some "sin" and repeatedly seeks you out for reassurance may have scrupulosity, a religiously themed form of obsessive-compulsive disorder. Don't take these and other behaviors personally. Learning about mental disorder symptoms is the first step of behavioral management.
Exercise astute observation. Be mindful, noticing subtle changes that may indicate emotional shifts. Be a student of body language and personal space. Awareness and flexibility can help you navigate with sensitivity a patient's unpredictable behaviors.
Firmly redirect inappropriate behaviors. It is a mistake to sidestep or tiptoe around patients whose behavior is disruptive. This not only reinforces the behavior but also, paradoxically, weakens your therapeutic bond. Stay grounded, speak calmly and be directive. With gentle but firm guidance, we can guard patients' dignity and help them self-regulate.
"Jeff" is a large man, towering well over 6 feet, but he has the attention span and impulsivity of a child. He is awaiting a hearing to determine if he is competent to stand trial and must be accompanied by security at all times. He is a regular participant in the spirituality group I facilitate and enjoys talking with me in the dayroom.
I'm in my office, just back from vacation, and can hear him at the far end of the corridor. "Chaplain Michele," he calls out excitedly, seeing me through the open door. Suddenly, he dashes down the hall and enters my office, slamming the door. Click. I hear the dead-bolt turning. Inexplicably, he has locked the door.
I hear security calling for backup. In a matter of seconds they'll be at the door. Standing up, I speak clearly, firmly and calmly: "Jeff, please unlock and open the door. NOW."
"Yes ma'am," he immediately replies, and complies with my directive. The crisis is averted, and Jeff is spared what likely would have been a humiliating, if not traumatizing, experience.
PATIENT SAFETY CONCERNS
A core and valued role of chaplains is to provide patients with requested religious or spiritual resources, as appropriate. We frequently are asked for sacred scriptures, rosaries, crosses, medallions and spiritual literature. But what if these resources, normally helpful for adaptive coping, pose safety concerns? How do we balance a patient's religious rights with treatment needs?
"Betty" is a Catholic patient with an extensive history of self-harm. When I first meet her, she asks for a rosary, identifying it as a primary source of comfort in her life. In consultation with the treatment team, however, I must deny the request. She has a history of ingesting objects. Instead, I explore with her creative ways to pray the rosary without use of beads.
Meanwhile, Betty contacts her parish priest and asks him for a rosary, complaining that the "uninformed" Protestant chaplain does not provide Catholic patients with this vital resource. Without contacting me, he complies with her request. Within days, Betty is rushed to surgery with a perforated colon: She has swallowed the rosary beads and the attached cross.
People with active mental disorders are at increased risk of self-harm and suicide. Remember that safety trumps everything, including use of religious resources. At times, even access to the Bible should be carefully monitored: Actively psychotic patients often take biblical passages literally and may act on distorted understandings.
Be especially vigilant about possible risks that come in the guise of spiritual concerns. Questions about suicide and hell are potent red flags, as they may indicate the patient is considering suicide, and the only remaining deterrent is fear of going to hell. Resist the urge to reassure and, instead, reinforce the concern. Make sure you notify the patient's physician or nurse, carefully documenting the conversation. These kinds of questions in behavioral health settings most often are a critical cry for help, not an occasion for compassionate theological discussion.
SIMPLE INTERVENTION STRATEGIES
The functional focus of behavioral health can empower our work as chaplains in many ways. Consider these simple strategies:
Explore the function of the dysfunction. Behavior often is purposeful, an attempt to meet needs or express what matters most. Even the most dysfunctional behaviors or puzzling illness symptoms may offer a window for understanding a patient's concerns, challenges, yearnings and needs.
"Jane" is a middle-aged woman who has been in and out of the hospital for most of her adult life. She is intelligent, caring and, when compliant with her medication, lives independently. Her behavioral pattern is consistent: Within weeks of hospital discharge, she stops taking her medication and quickly becomes incapable of self-care.
I see her sitting alone in the dayroom, laughing and talking as if engaged in lively conversation. I suspect she's hearing voices, a common symptom of her mental disorder. Spotting me, she waves and invites me to join her: Over time, we have developed a trustful rapport.
As I approach her, I mull over an intuitive hunch and decide to take a risk.
"Jane, I couldn't help but notice the conversation you were just having. You seemed so at home, like you were talking with old friends," I say.
Hesitantly, she replies: "You're right, I was talking with my friends, though most people say they aren't real. But to me they are very real."
I continue: "Is this why you don't like to take your medication?"
Jane's eyes well up with tears. In a barely audible voice, she says, "Yes, because when I take the medicine, my friends all go away. And they're the only friends I have."
Through the years I've found that spiritual assessment in behavioral health is an intuitive art. We listen for lucid moments in the midst of delusional talk. We look for nuggets of truth in the torrent of grandiose stories. We approach perplexing behaviors as possible pathways to meaning and purpose. And in so doing, we may very well get a glimpse of what matters most.
Look for the ability in the disability. In the fog of illness symptoms, it's easy to lose one's sense of self as a competent person. Over time, many fall prey to what disability rights advocate Patricia Deegan, PhD, calls "handicaptivity," the toxic belief that one is incapable of recovery. One of the greatest gifts we can offer patients is to help them rediscover their strengths and skills. By finding the ability in the disability, we can both motivate patients by eliciting their own capabilities and also identify internal spiritual resources.
Translate spiritual principles into concrete daily practices. Years ago, I completed an intensive training program in dialectical behavior therapy, the treatment of choice for working with difficult-to-treat patient populations, such as people living with borderline personality disorder. While there are many elements that make this cognitive-behavioral approach successful, what struck me most is its focus on practical skill development. It revolutionized my practice as a chaplain, especially in facilitating spirituality groups.
There are many ways to embed a functional focus into the provision of spiritual care. Teach basic spiritual practices (mindfulness, gratitude, forgiveness, prayer) as coping skills, breaking down each practice into concrete, doable steps. Facilitate values clarification, with a focus on aligning behaviors with core values. Present faith and hope as action verbs — spiritual truths that become felt realities as they are exercised. Identify specific ways to make meaning, connect with others, experience moments of joy. We empower patients' recovery by translating spiritual principles into teachable skills.
Always remember: There's a person in there. Early in my career, I was privileged to hear Deegan speak on recovery from mental disorders. An adjunct professor at the Dartmouth Institute for Health Policy and Clinical Practice, Deegan is a psychologist instrumental in the mental health paradigm shift from symptom management to recovery-focused treatment. She also lives with schizophrenia. Drawing from both her personal journey and a previous lecture, her remarks revolved around a simple theme: Remember, there's a person in there.
How do we best serve those living with mental disorders? We remember there's a person in there, a wonderfully made human being with goals, passions and dreams. We remember there's a person in there, loved by the Creator and created for community. We remember there's a person in there and help him or her remember too. And together in pursuit of re-membered wholeness, we embrace recovery, not as cure, but rather as stance in life, always resplendent in hope.
MICHELE J. GUEST LOWERY is an ordained minister in the United Church of Christ and a board-certified chaplain with the Association of Professional Chaplains. She has almost 20 years of experience in behavioral health chaplaincy as both a direct care provider and program coordinator. She currently serves as chaplain at Central Maine Medical Center in Lewiston, Maine.