BY: DEBORAH DAHL
 Bill (name changed to protect his privacy) is an educated, retired man with a history of multiple chronic conditions. He has coronary artery disease, diabetes, osteoarthritis, a pacemaker and has had a liver and kidney transplant. Last year, medical problems sent Bill to the emergency room six times and landed him in the hospital five times. As if that's not enough, he visits one of his many specialists every three or four weeks, followed by trips to the laboratory or imaging center for additional tests. Some days, he feels like managing his health is a full-time job.
Bill (name changed to protect his privacy) is an educated, retired man with a history of multiple chronic conditions. He has coronary artery disease, diabetes, osteoarthritis, a pacemaker and has had a liver and kidney transplant. Last year, medical problems sent Bill to the emergency room six times and landed him in the hospital five times. As if that's not enough, he visits one of his many specialists every three or four weeks, followed by trips to the laboratory or imaging center for additional tests. Some days, he feels like managing his health is a full-time job.
Based in Phoenix, Banner Health is a microcosm of health care in America. Twenty-five hospitals spread across seven Western states cover the delivery spectrum: critical access hospitals, urban teaching facilities, community hospitals and specialty hospitals. The nonprofit system comprises more than 200 clinics, a home health agency, ambulatory surgery centers, skilled nursing facilities and the 300,000-member Banner Health Network. Banner is growing, with new health plan members, new clinics and new hospitals joining.
In 2006, Banner began investigating telehealth by using 50 ICU beds to test the hypothesis that patients do better if there is a critical care physician (an intensivist) in every ICU, 24 hours a day, seven days a week. The hypothesis proved true, but the research pointed out a nationwide problem: The U.S. had only a fraction of the number of intensivists that would be needed to provide the traditional bedside physician model of ICU care all day, every day. Banner Health developed TeleICU as a way to deliver a critical care specialist to every bedside without having the physician on site.
Today, Banner's telehealth system manages 430 ICU beds in seven Western states. The intensivists describe TeleICU as doing rounds with their hands in their pockets. With two-way audio/video in every ICU room and Philips eICU™ software, the ICU's registered nurses and intensivists behind the camera can be proactive in delivering the best quality care. The tools can point out subtle changes in condition, give an alert for early signs of sepsis, and report opportunities for implementation of Banner Health's practice standards.
Medicine is a team sport, and the TeleICU program was not a replacement but an addition to Banner ICUs' bedside care staff, standard care protocols and checklists. Measurements with the health care industry's Acute Physiology and Chronic Health Evaluation (APACHE) tool show Banner Health's TeleICU has performed better than predicted in terms of ICU mortality, ICU length of stay and hospital stay for patients with some portion of their stay in the ICU.
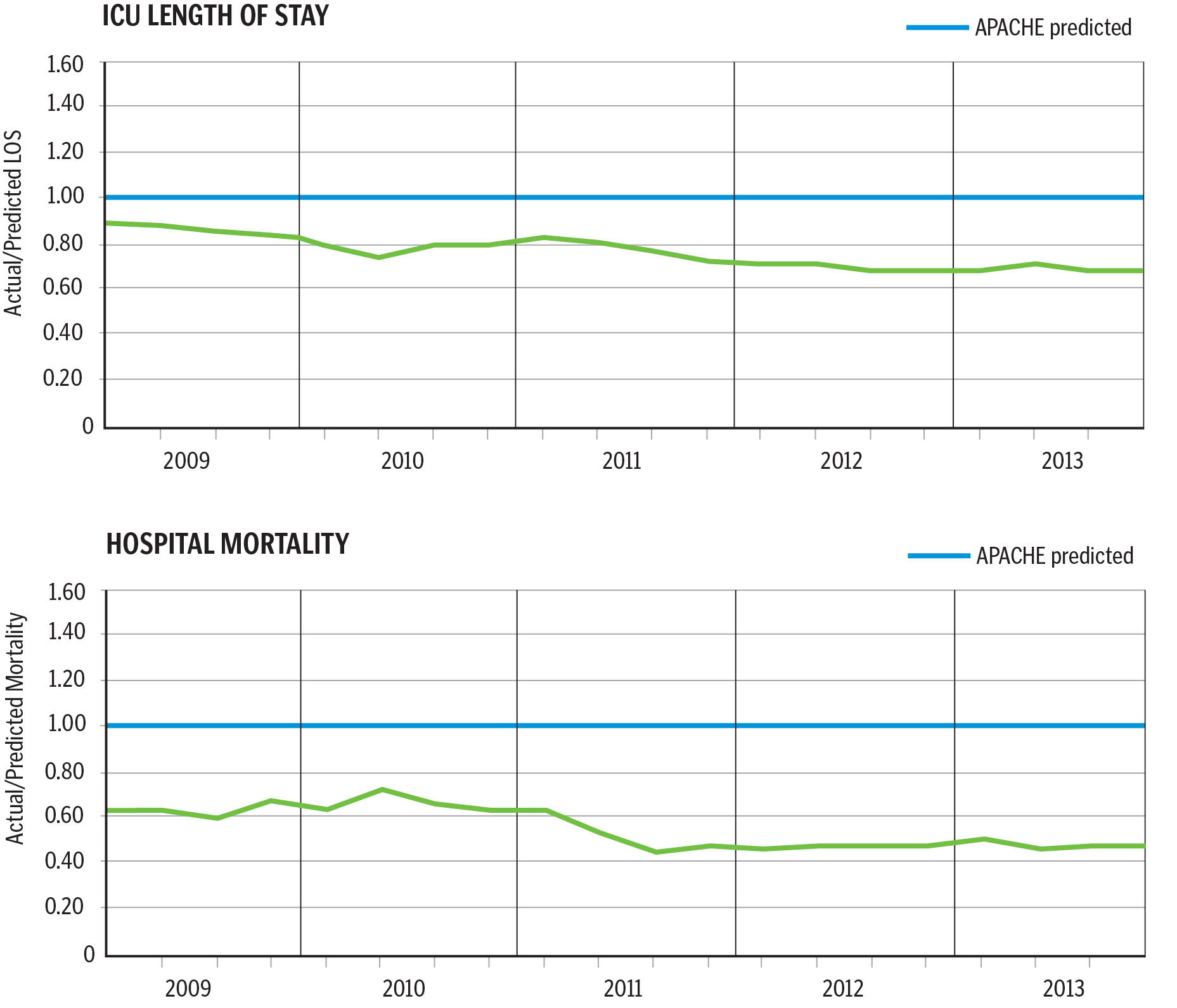
For 2013, the telehealth program trimmed more than 30,000 ICU days and more than 45,000 hospital days than statistically predicted and avoided $89 million in associated costs. But more importantly, the predicted mortality statistics changed, too: There were 1,890 fewer ICU deaths than statistically predicted.
Banner Health has successfully leveraged the ICU telehealth model into other areas of the hospital, including progressive care, medical/surgical, skilled nursing facilities and the emergency department, and it now offers specialty consultations such as neurology for TeleStroke, behavioral health, the Poison Center and wound management. These successes led Banner Health and its technology partner, Philips, to look beyond the hospital setting to the home.
iCARE
Historically, the U.S. health care system has focused on treating disease and reimbursing providers for the services rendered to patients like Bill. However, health care is moving to a model in which systems receive a fixed fee to care for populations of members, shifting focus away from acute care and toward maintaining their health. Simply put, treating disease is expensive; doing more is not always the best answer. Providing the right care, at the right time, in the right location, is the right answer.
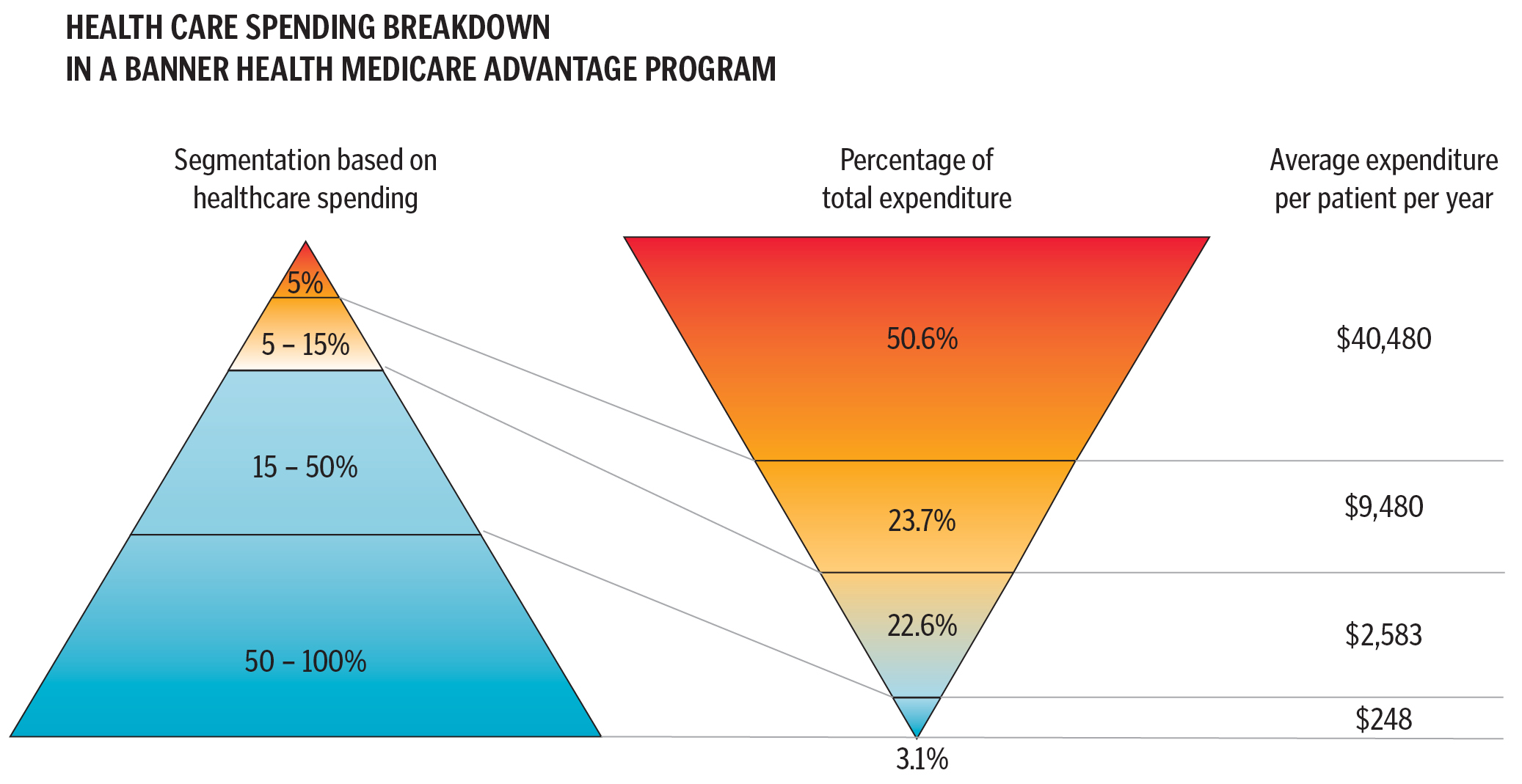
Banner Health has partnered with Philips to develop an innovative program called Banner iCare™ that specifically targets Banner health plan members who have multiple chronic diseases. Participation is limited to members with a history of high use of health care resources — the top 5 percent, who have average annual claims of $40,000-$50,000, account for 50 percent of the total cost of care.
The iCare program began in June 2013 in the retirement communities of Sun City, Sun City West and Sun City Grande, northwest of Phoenix, and began expanding across the Phoenix metro area in 2014. Participants belong to one of Banner's three capitated populations: Medicare Advantage plans, Banner employees enrolled in a medical plan, and members of the Pioneer Accountable Care Organization.
The technology, Philips eIAC™, is a comprehensive, remote monitoring and care management telecommunication program. Every iCare member receives a specially designed Philips tablet called "My Wellbook" that allows him or her to communicate with the Banner iCare team through two-way audio-video software and email. The tablet also delivers educational videos and surveys that collect information on member conditions beyond vital signs. The answer to a single question — "How are you feeling today?" — can be an indicator of overall emotional as well as physical health. Other questions look for changes in activity level, eating habits and cognitive ability.
The iCare members continue to see their primary care provider when they need in-person care, but for daily monitoring, they use the "My Wellbook" tablet along with in-home devices that measure blood pressure, heart rate, body weight and blood levels of glucose and anticoagulant medication. Sophisticated computer algorithms automatically assess this data and flag problems for the Banner iCare team to review; for example, worrisome changes in blood pressure or heart rate, failure to take needed medications or member survey answers that indicate worsening symptoms.
In this highly vulnerable population, an iCare member's condition can change rapidly. Registered nurses monitor the daily vital signs and check in with the member when changes occur. The nurses reinforce the plan of care, make suggestions for healthful behavior changes and provide education during the check-in exchanges.
Also behind the "My Wellbook" camera is a team of medical professionals, led by the iCare physicians. These clinicians are available for video consultation and support, and they assist with the medical plan of care and manage care transitions. They are the escalation point if a member's condition worsens.
Pharmacists perform medication reconciliation and identify high-risk states. They provide home monitoring of anticoagulation medication levels, assess medication regimes to minimize the risk of adverse drug events and promote member safety. They also serve as consultants for high-risk medication and disease state management. The pharmacist is available for member consultation and education regarding the state of his or her disease.
An important component of Banner iCare is its recognition that the environmental, social and emotional needs of its members and their families must be addressed. Issues like transportation, nutrition and other complexities of the health system often lead to patients' frustration and failure to meet goals.
The iCare team includes social workers who link members with community services — food banks or Meals on Wheels, transportation, support groups and financial services, for example. The iCare team also includes a social worker trained as a cognitive behavioral therapist, an amazing asset for a population in which many members suffer from depression or anxiety. Validated tools are used to determine depression and anxiety issues, and the social worker establishes trust and a therapeutic relationship while providing emotional support to the member and family, helping them to identify positive coping strategies.
A health coach on the iCare team is the program member's liaison — the first point of contact — and acts as a buddy. Certified nursing assistants by background, the health coaches are trained in motivational interviewing, learning phenotypes and member activation. Their primary role is to engage the member in managing his or her own health, and they start with a visit to the member's home for a safety check: Are there tripping hazards in the home? Is there mold in the ceiling? Is there appropriate food in the refrigerator? If problems exist, the health coach initiates a repair plan.
As the main contact person, the health coach concentrates on monitoring member safety, promoting lifestyle changes and recognizing and reporting changes in health status. Coaches have an eye for recognizing when members are not at peak performance and quickly connect them with the appropriate behind-the-camera clinician.
CHALLENGES
The health coach keeps in close contact, tracking whether a member has made a follow-up appointment as requested by his or her physician; attending a physician appointment with the member when requested; notifying the iCare pharmacist that a prescription has been changed. One of the greatest improvements for iCare will be integrating it into Banner Health's electronic medical record system so that the iCare team can quickly and easily see if the cardiologist changed a patient's medication or if another specialist has ordered a lab test.
However, even with the best of care, an iCare member may become a patient. When that occurs, the iCare team communicates with the urgent care center, emergency department or hospital to inform the medical staff there about the iCare member's conditions, medications and current plan of care.
Along with — and sometimes because of — the complexity of their health conditions, iCare members may not fully embrace their care regimen, which may result in clinical deterioration and the need for hospitalization. Among the many reasons for this behavior can be a lack of understanding of what is required, financial needs that take precedence over buying medicines, adverse drug reactions that members are uncomfortable discussing and complex emotional reactions to chronic illness that lead to dysfunctional behaviors.
In addition to using health coaches for education and support, Banner iCare uses a variety of strategies to reinforce successful behaviors. Considerable effort has gone into designing the "My Wellbook" tablet to link members with their iCare team and to provide continuous health information to positively impact the member's life. Banner Health's focus is to make the Banner iCare experience one that will enable and entice members to play a more active role in how they manage their health.
The Banner iCare program is designed to assist members in living a healthy, active lifestyle to the best of their ability. Most members enrolled in the program have a long history of frequent hospitalizations and ED visits, which is not optimal quality of life. Members often see a large number of medical specialists, take more than 10 different medications and endure many X-rays and blood tests. By providing proactive in-home care, Banner iCare will prevent hospitalizations and emergency department visits, reduce the number of specialist visits, simplify medication regimens and eliminate unnecessary and duplicative tests. And most importantly, members will have a better quality of life. Together, Banner and Philips are changing health care and improving the lives of members and their families.
Make no mistake; this change will not be an easy one. Health care has never really focused on maintaining health, lacking the systems, the people and the tools to do it. Success means recognizing that the population is heterogeneous, and one solution will not work for everyone. For healthy individuals without disease, the focus needs to be on disease prevention, which for many will entail lifestyle modifications. And for those who have stable medical conditions, the goal is compliance with prescribed therapies to slow disease progression and minimize acute flare-ups.
These two groups represent the bulk of the U.S. population, almost 95 percent. These individuals generally are fully functional and rarely need to access acute medical care. For them, improving health status will depend upon education, member engagement, perhaps some financial incentives and better support systems.
However the remaining population — approximately 5 percent of the U.S. population — suffers from multiple chronic diseases. These individuals are limited by their illnesses, they take many different medications and they require frequent medical care. This is the group for whom Banner iCare and Philips medical seek to improve the quality of life and reduce the total cost of care.
Bill enrolled in the Banner iCare program, in February 2014. His in-home technology includes a personalized tablet with two-way audio-video communication capability, electronic scale, blood glucose device and a blood pressure/heart rate monitor, all Bluetooth-enabled. His health coach, Candi, encourages him to take his measurements daily and to stay on track with his medications.
With the proactive work of the Banner iCare team, and Bill's dedication, Bill has had one visit to the ED in eight months, resulting in significant savings in the overall costs of his medical care and a major improvement in the quality of his life. He needs his strength to keep up with his wife, daughters, grandchildren and great-grandchildren. This summer, for the first time in years, he and his wife felt well enough to spend time at the family cabin in northern Arizona.
DEBORAH DAHL is vice president, patient care innovation, at Banner Health in Phoenix.