BY: LEONARD M. FLECK, Ph.D.
Given limited resources and a commitment by the Obama Administration to reform our health care system, how high a priority ought a just and caring society accord long-term care?
What I call the "just, caring problem" is central to health reform: What does it mean to be a "just" and "caring" society when we have only limited resources to meet virtually unlimited health care needs?1 If we cannot adequately meet all the health needs of patients in our health care system, how do we selectively meet needs in ways that are congruent with our sense of what a just and caring society ought to be? This is a problem of health rationing.
THE HEALTH CARE COST PROBLEM
The Patient Protection and Affordable Care Act has two main objectives: (1) improve access to needed health care for the 50 million uninsured Americans and roughly 25 million underinsured Americans, and (2) more effectively control health care costs so that access to needed health care is more affordable for all Americans. Over the past 40 years the average annual increase in health expenditures in the United States has been about 7 percent. That has resulted in health expenditures increasing from 5.2 percent of our GDP in 1960 to 17.6 percent of GDP in 2010. In 2010, total health spending was about $2.6 trillion. Projections to 2019, assuming the same growth trajectory, put total expenditures at about $4.5 trillion, 20 percent of expected GDP.2
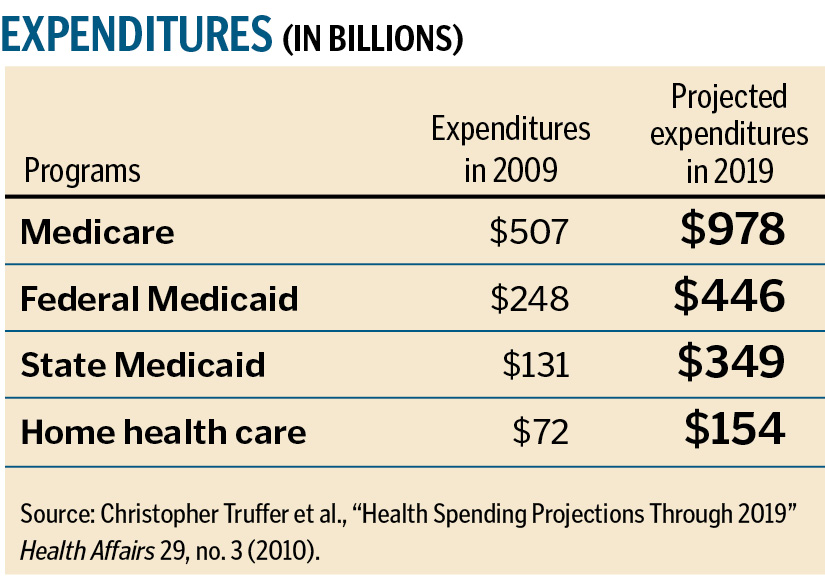
In 2009, Medicare expenditures were at $507 billion with projections to 2019 of $978 billion.3 Federal Medicaid expenditures were at $248 billion in 2009 with projections to 2019 of $446 billion.4 State Medicaid expenditures were at $131 billion in 2009 with projections to 2019 of $349 billion.5 Home health care in 2009 stood at $72 billion with projections to 2019 of $154 billion.6 Nursing home care in 2009 was at $144 billion with projections to 2019 of $246 billion.7
Many factors have contributed to the overall problem of escalating health care costs. The two most significant are expensive, emerging medical technologies and the growth of our elderly population. In 2010, the United States had about 40 million individuals over age 65, roughly 13 percent of the population. Projections to 2030 put our population over age 65 at about 80 million, or 20 percent of the population. The fastest-growing segment of the elderly population encompasses those over age 85, roughly five million people in 2005, expected to grow to almost 20 million by 2050.8
In 2010 about 1.6 million Americans over age 85 have moderate to severe memory impairment, with projections that number will increase to 6.2 million in the year 2050.9
This last statistic is very directly related to the torrent of new and expensive medical technologies, especially life-prolonging technologies, such as the array of heart medications, coronary angioplasties, implantable cardioverter defibrillators, left ventricular assist devices (for patients in end-stage heart failure) and, now in clinical testing, totally implantable artificial hearts. Further, complex life-prolonging surgery is now routinely done on patients in their 80s and 90s.10, 11, 12, 13, 14 But, as one writer has put it, we are "doing better and feeling worse."15 Patients are living longer but with a greater burden of chronic illness — more cancer, more (non-fatal) strokes, more arthritis, more sensory deficits and more cases of dementia. Roughly 23 percent of Americans over age 65 are now living with five or more chronic illnesses, and 62 percent have two or more chronic illnesses.16 "Feeling worse" is also about the increasing burden of costs associated with multiple chronic illnesses, both for taxpayers and the chronically ill.
THE LONG-TERM CARE PROBLEM
Most patients who are chronically ill are able to function with only occasional assistance from others. But many others need long-term care. That is, they have difficulty caring for themselves for at least 90 continuous days. About 12 million Americans needed long-term care in 2009, roughly 10 million in community settings and 1.8 million as nursing home residents.17 Of those nursing home residents, 1.6 million were over age 65. In the community setting, patients needing long-term care were roughly evenly divided between those above and below age 65.18
From an ethical perspective, what is noteworthy is that long-term care patients are generally among the medically and financially least well off. This would suggest that they ought to be among those deserving serious, high priority, moral attention for reasons of justice and compassion. But long-term care needs have been largely relegated to moral backwaters.
Long-term care patients are among the medically least well off because they generally have global permanent disabilities that require substantial assistance from others. They are a heterogeneous lot that includes individuals born with serious and varied developmental disorders, spinal-cord injuries, early adult disorders (such as multiple sclerosis), traumatic brain injuries, Parkinson's, stroke, and various sorts of dementias.
The medical needs of these long-term care patients may be reasonably well managed due to financing support from Medicare, Medicaid and some state and local funding. But long-term care needs are generally poorly funded and largely dependent upon being satisfied by the voluntary efforts of friends and family. Medicare funds very few long-term care needs.
In 2009, 44 million Americans assumed responsibility for attending to the long-term care needs of a friend or family member.19 That unpaid care has been valued at $350 billion. The quality of that care will vary enormously, largely because few of these caregivers have any formal training. In the case of the elderly, that informal caregiver is often a spouse with his or her own significant infirmities.
The Medicaid program spent about $220 billion (2009) for long-term care, most of that for nursing home care of impoverished individuals.20 In 2009, the average cost for a year in a nursing home was $78,000.21 Only a very small percentage of Americans have savings sufficient to pay for two years in a nursing home.
Likewise, only 10 percent of Americans over age 50 have some form of long-term care insurance, and most of those policies are of only marginal value.22 Most of those policies are very expensive for the middle class and quite complicated with regard to various policy limitations. In addition, the perceived need for such policies is very low, especially among middle-aged adults in very good health. Concerns also exist that the companies offering these policies might fail financially during the 30 or 40 years that intervene between the purchase of such a policy and the need to use it.
Finally, the cost of health insurance, including employer-sponsored health insurance, is diminishing any capacity the middle class might otherwise have to invest in long-term care insurance. The average cost for a family policy in 2011 is over $15,000.23 Most employers are expecting employees to pay a larger portion of that cost. The net result is that long-term care needs are poorly funded and poorly addressed.
LONG-TERM CARE PROPOSALS
The Obama Administration has been attentive to the inadequacies associated with long-term care. The Affordable Care Act originally included support for the CLASS program (Community Living Assistance Services and Supports), a voluntary, publicly administered insurance program. Given the need to control health care costs, especially governmental health care costs, the law required that this program be entirely supported by the premiums paid voluntarily (no federal tax dollars).
No one would be eligible to receive benefits from the program until they had paid into the program for at least five years. During at least three of those five years, individuals would have to have been actively employed (no set number of hours per week). The practical implication of this last point is that individuals already dependent upon long-term care could not just pay a monthly premium for five years and enjoy lifetime benefits from the program.
The monthly premium that individuals would have to pay would depend upon the age at which they joined the program. No other factor related to that individual could raise the cost of the monthly premium, including anything related to their past, present or predicted future health. From an ethical point of view, this is something worthy of praise. From an economic point of view, this appears to have been the Achilles heel of the program. Individuals whose earnings were below the poverty level would only have to pay $5 per month.
The basic benefit of the program, once an individual is judged as having trouble with at least two activities of daily living, would be $50 per day (adjusted for inflation). That money could be used for anything related to long-term care, including paying for home health aides, adapting a home for one's disabilities, residing in an assisted-living facility, nursing home expenses and so on.
That $50 per day might be largely sufficient for individuals whose long-term care needs could be met in a community setting with significant voluntary help, which is the setting much preferred by the vast majority of individuals needing long-term care. However, if nursing home care is necessary, that $50 would cover only a small fraction of daily expenses. Consequently, individuals would have to impoverish themselves to the degree required by Medicaid rules, at which point Medicaid would cover remaining expenses.
THE CLASS PROPOSAL
The obvious value of this program was that it addressed a very substantial unmet social need. Still, in October 2011, the Obama Administration was forced to abandon its commitment to long-term care, mostly for financial reasons.
Justice requires that the program be financially stable. That stability is defined as adequate funding for 75 years into the future. Medicare and Social Security can make and keep such promises because the programs are mandatory and federal funds can be used, if necessary, to cover any short-term funding deficiencies. But the CLASS program was intended to be entirely voluntary.
Given the political climate and a strong reaction against the individual mandate for personal health insurance, one would expect that the voluntary nature of the program would be a major advantage. That might be true, politically speaking, but it is likely false, practically speaking. Unless a major cultural change occurred in our society, the same factors that presently result in few healthy middle-class individuals being motivated to purchase long-term care insurance would likely undermine any actual commitment to the CLASS program as well.
The individuals who would be most motivated to take advantage of the program would be the poor and those who had good reason to believe they would need the benefits of the program in the not-too-distant future. This creates an "adverse selection" problem. If the vast majority of program participants have paid in very little but will withdraw a lot for many years, then premiums alone will not sustain the program.
The projected average monthly premium for the program was in the range of $123-$240 (much depending upon uncertain assumptions).24 But if the dominant early participants were the poor and long-term needy, as suggested above, then funds would be paid out more quickly than funds could come in. To rectify that imbalance, monthly premiums would have to be raised, perhaps substantially and unpredictably. Those higher costs would further erode the resolve of the healthy middle class to join the program.
A number of other adjustments could be made to the CLASS program as it had been envisioned to produce fiscal stability. The minimal vesting period could be raised to 10 or 20 years. Individuals could be required to work 20 or 30 hours per week during most of that period. Participation in the program could be mandated. Large financial penalties could be imposed on those who dropped out of the program and later sought to re-enroll. The benefit period could be restricted to a set number of years rather than the rest of one's life. Individuals could be required to have a higher level of disability before they became eligible for benefits.25
All the adjustments proposed above might well result in a more financially stable program, but the political, practical and ethical costs would be substantial. Mandated participation in the political climate would be the proverbial deal breaker. Lengthening the vesting period for 20 years would mean the Baby Boom generation would be effectively excluded as potential beneficiaries (and financers) of the program. Given the size of this generation (80 million), and given the likelihood of various degrees of their long-term needs (70 percent will have some long-term need before death), failure to address those needs would be ethically problematic.
Limiting the scope of benefits and penalizing individuals for dropping out for some period of time (perhaps as a result of a long period of unemployment or other extraordinary family expenses, such as a health crisis) would create strong disincentives for not joining the program at all or waiting until very late in one's working life.
THE PRIORITY-SETTING CHALLENGE
What should we, citizens in a society aspiring to be just and caring, do, especially when we have only limited resources to meet virtually unlimited health care needs? First, we need to answer this question as an ethical question; then we need to do considerable creative social thinking to design innovative approaches to meeting long-term care needs. Those designs would then determine the financing scheme needed to support that design.
The ethical challenge. As I have argued elsewhere, 26, 27 we have to be willing to accept limits on access to needed health care, and this in turn will require our making trade-offs and setting priorities among a large and diverse range of health care needs. This is the challenge of health care rationing. It is an ethical challenge because these difficult choices must be made in ways that respect our shared sense of what a just and caring society ought to be.
Though health care rationing is the focus of considerable political obloquy and disingenuousness, it is not something that is intrinsically ethically objectionable. Rationing is ethically objectionable when such decisions are imposed on the sick, the weak, the poor and the politically vulnerable by the wealthy, the healthy and the politically powerful. This violates the equal concern and respect that we owe one another.
Rationing is also ethically objectionable when such decisions are effected in ways that are hidden from public scrutiny. Relying upon individual ability to pay for needed care to determine who actually receives health care is one such hidden form of rationing. What is hidden from public scrutiny is whether or not that instance of rationing is just. As Rawls has put it, when policies and practices are just, nothing needs to be hidden.28
The need for democratic deliberation. Rationing decisions are more likely to be just when they are self-imposed through a public and inclusive process of rational democratic deliberation. I can only sketch here what I have elaborated more fully in my book.29 First, the process must be public and inclusive. It is a common pool of resources that must be accessed to meet our health care needs, whether a private insurance plan or Medicare. Individuals as individuals have no just claim to access anything and everything our health care system has to offer at someone else's expense. What will count as "just" will depend upon the agreements we freely reach through the deliberative process.
Second, the deliberative process must be rational. We have to rely upon the best medical and scientific evidence available at a point in time, and we must be able to give reasons to one another for any particular rationing proposal that all can endorse as reasonable. This preserves equality of respect for all in similar medical circumstances. Thus, if I believe Mr. Smith, an 85-year-old individual with end-stage Alzheimer's and signs of a potentially fatal arrhythmia, does not deserve a $40,000 implantable cardioverter defibrillator to prevent that arrhythmia at social expense, then I must be willing to say in the same breath that if I were in those same circumstances in the future, I, too, would not deserve that implantable defibrillator. Likewise, if I believe that it would be a poor use of limited health care dollars (my insurance dollars) to provide a $100,000 cancer drug to 63-year-old Jane Doe with an end-stage cancer for six extra weeks of life, then I must be willing to say the same about a future possible version of myself in those same circumstances (and wanting to use your insurance dollars).
Third, the deliberative process must be impartial. Critics of public deliberation believe such impartiality is impossible to achieve because self-interest and interest-group politics commonly corrupt legislative deliberation. But that is because individuals intimately know their own interests. This is rarely true in the health care context. The vast majority of us are quite healthy most of the time. We are largely ignorant regarding our future possible health needs. We are literally behind what Rawls has dubbed a "veil of ignorance."30 Even if I know I am genetically vulnerable to heart disease, I do not know which of hundreds of other medical problems I might be vulnerable to as well. This is what allows all of us to judge more fairly what our collective health priorities ought to be when we have only limited funds for meeting the full range of our health care needs. In addition, each of us has a large circle of family members and friends, often spanning several generations, whose diverse health needs will be as important to us as meeting our own needs. Being reminded of that fact also reinforces our capacity for making impartial health care priority judgments.
CRITICAL QUESTIONS
Here are the kinds of questions we need to ask ourselves in the deliberative process: Is it more important (just and caring) to underwrite with Medicare dollars access to left ventricular assist devices or totally implantable artificial hearts for individuals over age 80 in end-stage heart failure, or should those tens of billions of dollars be used to underwrite a broad range of community-based, long-term care services?
The same question needs to be raised with regard to these $100,000 cancer drugs that promise no more than extra weeks or extra months of life.31, 32
We fear cancer; we fear death. Should we not also fear long-term dependency and the demands this will make upon friends and family in the absence of a well-planned, long-term care program?
Critics might charge that what is being proposed here represents age-based rationing, ageism, a form of discrimination that should be as morally obnoxious as racism. However, the charge of ageism can go two ways. As things are now, the Medicare program permits the elderly to demand as a matter of right virtually anything the health care system has to offer, no matter how high the cost, no matter how minor the benefit. This is what will drive the Medicare program to the trillion-dollar level by 2019. Unlimited costly demands such as that will undermine the capacity of the Obama Administration to secure access to needed and effective basic health care for the younger uninsured in our society. Surely this should be regarded as a form of unjust discrimination as well.
We (the near-elderly) also need to ask ourselves whether we are willing to take more responsibility for our own health. Specifically, are we willing to undertake a serious exercise program and pay closer attention to a healthy diet in order to reduce the future health costs associated with diabetes and heart disease and some cancers? Again, do we believe it would be either just or responsible to pass the costs of our casual unhealthiness to the generation behind us in the form of higher Medicare taxes? Likewise, do we also believe that we would have a just claim to long-term care services paid for by the generation behind us when we ourselves are unwilling to sacrifice any very costly, marginally beneficial health care services?
If individuals truly dread spending their last months and years of life in a nursing home in end-stage dementia,33 and if individuals strongly prefer getting good quality care in a community setting by trained caregivers (as opposed to making extraordinary demands upon friends and family who are ill-prepared to offer the level of care needed),34 then perhaps we ought to come to a collective social understanding that we will refuse in advance social funding for any sort of life-sustaining care at all for our future possible selves in the end stages of dementia, including artificially provided food and fluids.35
The proposals suggested in the prior paragraphs would literally save tens of billions of dollars per year, if we would collectively agree to them. We should not kid ourselves. Those are the kinds of resources that would be necessary to have high quality long-term care resources provided in the community.
INNOVATIVE RESPONSES
A number of creative experiments in such community care have been tried and have demonstrated substantial success. Gleckman describes a number of NORCs (Naturally Occurring Retirement Communities) in various parts of the country that have been successful.36 He also describes the "Village" experiments tried in Beacon Hill in Boston and around Capitol Hill in Washington, D.C.37 There are also the PACE experiments (Program of All-inclusive Care for the Elderly), one of which was attached to Johns Hopkins Bayview Medical Center in Baltimore.38 All these programs provide high quality, comprehensive long-term care to mostly elderly individuals in a community setting. They substantially reduce demands on friends and family, but they are costly. Given the demise of the CLASS program, these alternatives take on even more importance.
If such programs are to become widely available in the United States, then they would need stable funding. Such funding is unlikely to be achieved through the voluntary purchase of insurance products. The backing of the federal government would be essential. That in turn means enrollment in the program would be mandatory, as with Medicare. This might be more readily accomplished, politically speaking, if such a comprehensive community-based care benefit were integrated into Medicare.
Taxpayers would (presumably) not want to see the Medicare portion of the Social Security tax rate increased. This is not unreasonable. But then taxpayers would have to endorse for their future possible selves the trade-offs and rationing protocols proposed above. If the near-elderly truly do not wish to be a burden to friends and family, either economically or socially, then the trade-offs suggested above ought to be endorsed.
Ethically speaking, a just and caring society ought to be responsive to the health care needs of those who are "least well off" health-wise. But it is far from ethically obvious that the correct implementation of that directive requires artificial hearts, left ventricular assist devices and extraordinarily expensive, marginally beneficial cancer drugs. Not a lot of care is built into an artificial heart. But a lot of care can be built into a properly designed, comprehensive, community-based long-term care program. At the very least this option deserves a thoughtful and respectful public conversation.
LEONARD M. FLECK is a philosophy professor and faculty member in Michigan State University's Center for Ethics and Humanities in the Life Sciences, East Lansing, Mich.
NOTES
- Leonard M. Fleck, Just Caring: Health Care Rationing and Democratic Deliberation (New York: Oxford University Press, 2009).
- Christopher J. Truffer et al., "Health Spending Projections Through 2019: The Recession's Impact Continues," Health Affairs 29 (2010): 522-29.
- Truffer et al., 525.
- Truffer et al., 525.
- Truffer et al., 525.
- Truffer et al., 525.
- Truffer et al., 525.
- U.S. Census Bureau, Statistical Abstract of the United States: 2000 (Washington, D.C.: U.S. Census Bureau, 2000), at www.census.gov/prod/2004pubs/ (accessed Sept 30, 2011).
- Family Caregiver Alliance: National Center on Caregiving, Fact Sheet: Selected Long-Term Care Statistics, at www.caregiver.org/caregiver/jsp/print_friendly.jsp?nodeid=440 (Accessed Sept. 30, 2011).
- W. Michael Johnson et al., "Cardiac Surgery in Octogenarians: Does Age Alone Influence Outcomes?" Archives of Surgery 140 (2005): 1089-93.
- Philipp Geisbusch et al., "Endovascular Repair of Infrarenal Aortic Aneurysms in Octogenarians and Nonagenarians," Journal of Vascular Surgery 53 (2011): Epub ahead of print, www.ncbi.nlm.nih.gov.proxy1.cl.msu.edu/pubmed/21908147 (Accessed Sept. 30, 2011)
- Lee J. Goldstein et al., "Endovascular Aneurysm Repair in Nonagenarians is Safe and Effective," Journal of Vascular Surgery 52 (2010): 1140-46.
- Miralem Pasic et al., "Transapical Aortic Valve Replacement Implantation in 175 Consecutive Patients: Excellent Outcomes in Very High-Risk Patients," Journal of the American College of Cardiology 56 (2010): 813-20.
- Christoph H. Huber et al., "Benefits of Cardiac Surgery in Octogenarians: A Postoperative Quality of Life Assessment," European Journal of Cardio-Thoracic Surgery 31 (2007): 1099-1105.
- Aaron Wildavsky, "Doing Better and Feeling Worse: The Political Pathology of Health Policy," in Doing Better and Feeling Worse: Health in the United States, edited by John Knowles (New York: W.W. Norton, 1977): 105-24.
- Christine Vogeli et al., "Multiple Chronic Conditions: Prevalence, Health Consequences, and Implications for Quality, Care Management, and Costs," Journal of General Internal Medicine 22 (supplement 3)(2007): 391-95.
- Joanne Kenan, "Health Policy Brief: The CLASS Act," Health Affairs (May 12, 2011): 1-6.
- Kenan, 1-6.
- Howard Gleckman, Caring for Our Parents (New York: St. Martin's Press, 2009), ix.
- Truffer et al., 523.
- Gleckman, x.
- Gleckman, x.
- http://money.cnn.com/2011/09/27/news/economy/family_health_insurance_cost/index.htm (Accessed Oct. 1, 2011).
- Kenan, 4. She cites the Congressional Budget Office, the Boston College Center on Retirement Research, and actuaries for Medicare and Medicaid as sources for these estimated monthly costs.
- Kenan, 4-5. All the proposals mentioned in this paragraph are identified by Kenan as options.
- Fleck, 2009.
- Leonard M. Fleck, "Just Caring: Health Care Rationing, Terminal Illness, and the Medically Least Well Off," Journal of Law, Medicine & Ethics 39 (2011): 156-71.
- John Rawls, Political Liberalism (New York: Columbia University Press, 1993): 3-46, 66-71 (stressing the idea that society must be a fair system of cooperation and that the "publicity condition" is at the core of our shared sense of justice).
- Fleck, 2009: Chapter Five.
- John Rawls, A Theory of Justice (Cambridge, Mass.: Harvard University Press, 1971).
- Tito Fojo and Christine Grady, "How Much is Life Worth? Cetuximab, Non-Small Cell Lung Cancer, and the $440 Billion Question," Journal of the National Cancer Institute 101 (2009): 1044-48.
- Eric Nadler et al., "Do Oncologists Believe New Cancer Drugs Offer Good Value?" The Oncologist 11 (2006): 90-95. Nadler noted that the implied cost-effectiveness for bevacizumab was $300,000 per Quality-Adjusted Life Year, a figure that only 25 percent of oncologists thought was a "good value."
- Gleckman. See the numerous stories he presents throughout this thoughtful volume.
- Jane Gross, A Bittersweet Season: Caring for Our Aging Parents — and Ourselves (New York: Knopf, 2011). Gross presents three poignant vignettes at the beginning of this volume of three very old women who needed intense amounts of care from their adult children. She comments, "These three strong-willed old women were grateful for their children's devotion but resistant to giving up the reins. They were embarrassed by their own diminished capacity and frightened of what lay ahead, but nothing was worse, they said, than being a burden."
- It is easy to imagine death panel rhetoric being hauled out here. However, no one would be absolutely denied any of these expensive, life-prolonging technologies. Individuals who so wished could pay for these technologies themselves or through insurance products (if offered). As long as such purchases are not publicly subsidized in any way, there is no injustice. Such purchases make no one else in the health care system less well off, nor do they violate any rights.
- Gleckman, 119-22.
- Gleckman, 122-24.
- Gleckman, 164-70.
Copyright © 2012 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.