BY: REV. ADAM RUSSELL TAYLOR
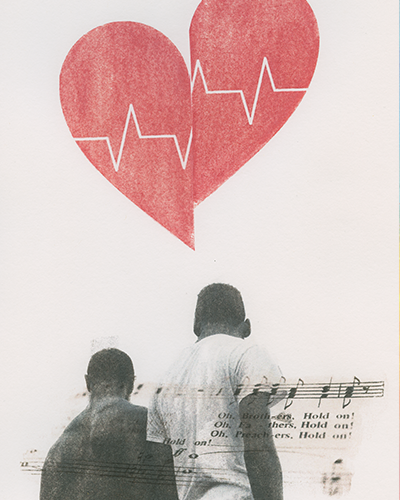
Illustration by: Jen Everett
Abundant life. Human dignity. A seamless garment of life. All of these sacred promises and commitments are at the very heart of the Christian faith and form an ethical standard to guide and measure public policy and leadership around the elements of the common good, including health care. Yet these faith imperatives are being undermined and betrayed by pervasive and persistent racial disparities in health care, many of which are tied to the legacy and continued impacts of institutionalized racism. The COVID-19 pandemic has further laid bare the dire consequences of entrenched systemic racism and injustice within our society and health system with African Americans being disproportionately infected and killed by the virus at alarming rates.
When I think about racism, health care and the well-documented disparities in health outcomes, three closely related but distinct perspectives are paramount. First is a historical perspective, which must include the ongoing legacy of the transatlantic slave trade that began over 400 years ago. America's original sin of slavery has contributed directly to a multitude of inequities in health care and health outcomes, many of which persist to this day. Second is a sociological and political perspective that can help us better understand the ongoing impacts of racial bias and institutionalized racism. Third is a theological and religious perspective, which starts with the Gospel mandate to ensure that every person, each of whom is literally made in God's image, can experience life in all its fullness. This requires achieving true equity in our health system and dismantling institutionalized racism.
The legacy of health care policy in the United States is deeply entwined with the legacy of slavery through Jim Crow segregation, and the disparities we see today cannot be properly understood without integrating this crucial context. Jeneen Interlandi has noted that, in the aftermath of the Civil War, when camps of newly emancipated people were being ravaged by smallpox and other diseases across the post-war South, "white leaders were deeply ambivalent about intervening. They worried about Black epidemics spilling into their own communities and wanted the formerly enslaved to be healthy enough to return to plantation work. But they also feared that free and healthy African Americans would upend the racial hierarchy..."1 She goes on to note that even as Congress created a program to provide health care to newly emancipated people, the program was chronically understaffed and under-resourced.
After Reconstruction, discriminatory policies and practices under Jim Crow became at least as prevalent and tenaciously embedded in the health care sector as any other part of society. Hospitals and medical schools were segregated, the American Medical Association (AMA) barred Black doctors from membership, and "access to good medical care was predicated on a system of employer-based insurance that was inherently difficult for Black Americans to get."2 When the National Medical Association (the leading Black medical society) began to fight to end segregation in health care, they had to contend with fierce opposition from the AMA, which used familiar arguments to defeat proposals for national health care programs in the 1930s and '40s: "...they called the idea socialist and un-American and warned of government intervention in the doctor-patient relationship."3 It was only with the passage of the Civil Rights Act and the bills that created Medicare and Medicaid in the 1960s that legal segregation in hospitals came to an end.
The provocative New York Times' "1619 Project" describes how many of the inequities that Black people experience in treatment by health care providers in the United States can be traced back to slavery, including the harmful beliefs that arose to justify slavery by falsely ascribing physiological differences between Black and white people.4 Some of these myths — most notably the belief that Black people don't feel pain to the same degree as white people — found their way into the scientific consensus and remain deeply embedded in the implicit bias of many health care providers. For example, a 2016 a study of white medical students and residents found that "half of [those surveyed] endorsed at least one myth about physiological differences between Black people and white people, including that Black people's nerve endings are less sensitive than white people's."5 Implicit or explicit biases like these contribute to the inequities we see across the U.S. health care sector, where research has shown that white people receive more and better pain treatment than Black people, despite their experience of similar levels of pain.6
Beyond the biases passed down from the era of slavery through Jim Crow segregation to the present, there are also egregious examples of racism in health care, such as the infamous Tuskegee experiment. The "experiment" had nearly 400 Black men with syphilis observed by the government while treatment was withheld (unbeknownst to the patients) for 40 years until it was exposed by a whistleblower in 1972. Some of the men in the study died, others went blind or suffered severe mental illness, and at least 40 spouses and 19 infants were infected due to the U.S. government's use of human research subjects in such a profoundly racist and morally abominable fashion.7 The exposure of the project in 1972 and subsequent coverage in the national press fed a profound mistrust of government and health care professionals that many Black Americans feel to this day.
The inequities in medical care combine with other forms of structural racism to create deep disparities in health outcomes for Black and white Americans. One of the best known is the difference in the rates of infant and maternal mortality between white and Black mothers and babies. According to Dwayne Proctor of the Robert Wood Johnson Foundation, "as recently as 2015, Black babies are more than twice as likely as white babies to die before their first birthdays" and "Black mothers in the United States die at 3 to 4 times the rate of white mothers."8 Among all ethnicities in the United States, African Americans have some of the worst child health indices including: 2.89 percent very low birth weight babies; 13.4 percent preterm live births and 3 percent of live births born before 32 weeks gestation. Based on the overwhelming science that shows how a lack of early childhood development stunts and sabotages kids physically and mentally, African Americans disproportionately have the odds stacked against them in health factors that impact the rest of their lives.9 Dr. James Lee, an African-American Catholic who leads an orthopedic practice that serves many underprivileged communities across the greater Newark area, argues that "while evidence shows that Black patients who have Black doctors tend to have better health outcomes, there has been an alarming trend in which Black men in particular are not going into the medical profession."10
The causes of health disparities are complex. At the least, they include a combination of the structural and economic inequalities that create gaps in quality of care, especially in putting Black mothers and infants at greater risk, the documented bias that some Black people face from some medical providers; and the cumulative strain associated with being Black in America.11 Another disparity linked to these cumulative and interconnected factors is the fact that Black Americans between the ages of 18 and 49 are twice as likely to die of heart disease as their white counterparts.12 The end result of these and other disparities is that life expectancy for Black Americans in 2014 was 75.6 years — on par with the life expectancy achieved for white Americans more than 30 years ago in 1987.13
When I reflect on the health experience of my mother's side of the family, I can't help but think that lack of access to health care and distrust of the health system played some role in the early deaths of my beloved uncle Danny and my grandfather Russell, from whom I got my middle name. Like many men of his time, my grandfather was a prodigious smoker, going through over a pack a day of his favorite Camel cigarettes for too many years and before the scientific evidence of the perilous harm of smoking was widely known. Russell raised his family in segregated Louisville, Kentucky, where access to preventive care and diagnostics was limited for Black families. While Russell regularly saw his Black family doctor and eventually did quit smoking, it was too little too late, as too much damage had already been done to his heart. He died at age 54. As a result, I never had the honor of meeting my grandfather.
My mother's younger brother, Uncle Danny, died of prostate cancer at the age of 66. I still remember him as being so fit and seemingly invincible as an accomplished athlete who still owns a rushing record at Oklahoma State University. My uncle's struggle with prostate cancer was complicated, due in some part to his own denial about the severity of his symptoms, but also due to his lack of access to consistent and quality health care as a self-employed businessman. I can't help but believe that his late diagnosis and treatment were tied in part to barriers within the health care system, his own suspicions of institutional health care and his lack of coverage. By the time he could access Medicare at age 65, which helped cover the cost of his care and hospitalization, his cancer was too far advanced and he died the next year.
As a Christian, it is impossible for me to look at the racial inequities in this nation's health system and not feel compelled to advocate for bold reforms and to fight for a radically more just health system as an imperative of my faith. The changes we must seek to make will have to come at both the societal and the individual levels — in our national, state and local policy decisions, but also in our hearts, choices and priorities. Followers of Jesus, along with others of faith and conscience, are called to work at both of these levels, just as Sojourners — the organization I help lead — has always believed. I'm deeply grateful that I work for an organization that lives out and prioritizes a commitment to physical, mental and spiritual health by providing full health insurance at no added cost to its employees and their families.
My social ethics and theology owe a great deal to Catholic social teaching, which has shaped the lens through which I see our broken health care system and ongoing disparities in health care. Catholic principles of solidarity, seeking the common good, subsidiarity and human dignity provide a moral compass to guide policy and anchor our political priorities, including those about health care. First, if we believe that all human beings are created in the image of God and bear God's image (Gen. 1:27-28), then all people should be equally entitled to basic human rights like life, freedom and health, not to mention dignity and respect. Seen in that light, it should be clear that health equity is just as important a pro-life issue as war and peace, the death penalty and even abortion. If all lives are sacred, at every stage of life, then the lives of Black mothers and Black babies in their first year must be just as important to us as all other lives — and it must be unacceptable to Christians that these lives are so much more often cut short than those of other mothers and babies.
We also can't ignore the connection between poverty and health care. The Bible and more than 2,000 years of Christian teaching have passed on to us the reality of God's preferential option of caring for the vulnerable and the poor. For example, Catholic social teaching, as articulated in the Compendium of the Social Doctrine of the Church, lists health care as a human right along with food, housing, work, education and transportation. The Compendium also specifies that "those without health care" are among those who should receive preferential consideration in the personal and structural decisions we make.14 Like so many of his predecessors, Pope Francis echoes this core belief saying that "Health is not a consumer good but a universal right, so access to health services cannot be a privilege"15 This simple but profound principle is fundamental to transforming and creating greater equity within our health care system.
Another foundational text for understanding Christian discipleship in the context of health care is Chapter 25 of Matthew's Gospel. There the disciples are told that "whatever you do for the one of the least of these brothers of mine, you did for me." If we believe that how we treat someone who is sick is how we treat Jesus himself, then it is not enough to say prayers or bring soup to a sick neighbor or fellow parishioner. We must also change policies and systems so that all who find themselves sick have an equal opportunity to get well again, even to have the same opportunity to be and remain healthy in the first place. Furthermore, as Sojourners founder Jim Wallis notes in his most recent book Christ in Crisis, the parable of the Good Samaritan (Luke 10: 25-37) teaches us that it's precisely those who are unlike us who are our neighbors, and that we have a duty to treat them the way we ourselves want to be treated.16 By working from the perspective of and in solidarity with the marginalized and most vulnerable, we demonstrate in our deeds both our love of God and our love of our neighbors as ourselves.
Racism in health care is a like a cancer that has evolved and often metastasized through attitudes, systems and structures. The COVID crisis can serve as the long overdue wake-up call and tipping point that inspires and forces us to finally remove this cancer. While there is no single cure, we must apply a series of effective treatments that include building greater trust in health care institutions and practitioners, increasing access to affordable and quality care and coverage, improving the cultural competency of health care providers and increasing the number of African-American doctors and providers. While racism in health care has become less overt, it still exists and is harmful both to the body of Christ and to people's individual health. As the Apostle Paul teaches us in I Corinthians 12, "when one part of the body suffers, all parts suffer with it." Our nation and the church at large will continue to suffer as long as racial disparities in health care persist. It is time for us to faithfully provide these and other treatments to ensure that every one of us can experience abundant life and human dignity.
REV. ADAM RUSSELL TAYLOR is the executive director of Sojourners and author of Mobilizing Hope: Faith-Inspired Activism for a Post-Civil Rights Generation.
- Jeneen Interlandi, "1619 Project," The New York Times, Aug. 14, 2019, https://www.nytimes.com/interactive/2019/08/14/magazine/universal-health-care-racism.html.
- Interlandi, "1619 Project."
- Interlandi, "1619 Project."
- Linda Villarosa, "1619 Project, The New York Times, Aug. 14, 2019, https://www.nytimes.com/interactive/2019/08/14/magazine/racial-differences-doctors.html.
- Villarosa, "1619 Project."
- Ronald Wyatt, "Pain and Ethnicity," AMA Journal of Ethics website: https://journalofethics.ama-assn.org/article/pain-and-ethnicity/2013-05.
- "Tuskegee Experiment: The Infamous Syphilis Study," History.com website, https://www.history.com/news/the-infamous-40-year-tuskegee-study.
- "New Narratives of Hope: This Black History Month — And Beyond," Robert Wood Johnson Foundation Culture of Health Blog, Feb. 5, 2020, https://www.wjf.org/en/blog/2018/02/new-narratives-of-hope-this-black-history-month.html?rid=0034400001nD3TmAAK&et_cid=1980396.
- Ifeanyi M. Nsofor, "Institutionalized Racism Is Keeping Black Americans Sick," The Hill, May 13, 2019, https://thehill.com/opinion/healthcare/443455-institutionalized-racism-is-keeping-black-americans-sick.
- Phone conversation with James Lee, MD.
- Zoe Carpenter, "What's Killing America's Black Infants," The Nation, Feb. 15, 2017, https://www.thenation.com/article/archive/whats-killing-americas-black-infants/.
- "African Americans Impacted More By Some Diseases," KARE11 website, Feb. 6, 2020, https://www.kare11.com/article/news/health/healthfair-11/health-disparities/89-011459f5-ae7d-41a1-917d-3bcf692d9ebe.
- Laura Santhanam and Megan Crigger, "New Report Reveals Persistent Health Disparities By Race in the U.S.," PBS Newshour, April 27, 2016, https://www.pbs.org/newshour/health/new-report-reveals-persistent-health-disparities-in-the-u-s. See also "New Narratives," RWJF Culture of Health Blog.
- Robert David Sullivan, "What Does Catholic Social Teaching Say About the GOP Health Care Plan?," America, March 10, 2017, https://www.americamagazine.org/politics-society/2017/03/10/what-does-catholic-social-teaching-say-about-gop-health-care-plan.
- Cindy Wooden, "Health Care Is a Right, Not a Privilege, Pope Says," Catholic News Service, May 9, 2016, https://www.catholicnews.com/services/englishnews/2016/health-care-is-a-right-not-a-privilege-pope-says.cfm.
- Jim Wallis, Christ in Crisis: Why We Need to Reclaim Jesus (San Francisco: HarperOne, 2019), 23-30.