BY: EDEN TAKHSH, MD; JAMES SIFUENTES and GENESSA SCHULTZ, EdD
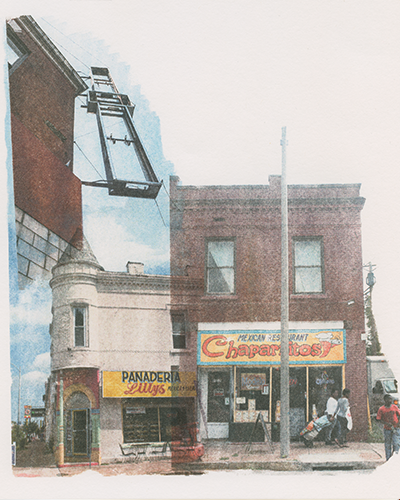
Illustration by: Jen Everett
At Saint Anthony Hospital in Chicago, our Catholic mission and values focus our work on meeting the needs of the underserved. Our vision aligns with what Jesus told his followers: "whatever you did for one of the least of these brothers and sisters of mine, you did it for me." (Matthew 25:40) Due to historically racist systems and policies in the United States, "the least of these" often end up coming from oppressed communities of color. Racist and oppressive policies manifest in the form of implicit bias, poor quality of health care, high cost of services and stereotypes that directly affect how people of color utilize health care systems, often waiting until symptoms, illnesses and diseases become detrimental to their health before seeking medical care.1 The need for trusted and quality care provided by safety net hospitals in marginalized communities is vital in improving health outcomes. Saint Anthony is a safety net hospital.
As providers and hospitals try to meet the needs of people within communities serving marginalized populations largely made up of African American and Latino people, unnecessary obstacles to providing quality care continue to get in the way. Fiscal obstacles are among the largest and most difficult to overcome. The incorporation of for-profit Managed Care Organizations, or MCOs, created to distribute funding to hospitals and providers for the Medicaid population, have detrimentally impacted how hospitals, specifically safety net and critical care hospitals, receive payment for services provided to marginalized populations. Saint Anthony Hospital is one of many safety net hospitals grappling with budgetary concerns when we'd like to instead be more focused on meeting the health care needs of our communities.
Since 1896, Saint Anthony Hospital has served people on the West and Southwest sides of Chicago, which have historically consisted of high need, immigrant populations. Currently, Saint Anthony Hospital's primary service area includes predominantly African American, Latino and Asian populations. In our service area, 23% to 45% of residents are living below the national poverty level; the children in this population make up 31% to 59% of those living in poverty.2
In keeping with our mission, we not only serve our community, we provide a high level of quality care. In fact, based on the Illinois Hospital Association's most recent data, we are in the top 10th percentile for patient safety and cost-effective care in Illinois, the top 10th percentile for patient safety nationally, and the top 20th percentile nationally for total performance score, which combines quality, cost and patient experience. We received the Illinois Hospital Association Innovation award in 2018 and 2019 and have been named a "Best Value" hospital in Chicago when costs are compared with quality scores.3
Our commitment to high quality care comes at a price which, up until 2017 when for-profit MCOs were created to deliver payments to providers, has been a commitment we were able to maintain by careful stewardship of limited resources. When a patient comes in, our hospital provides high quality care to the patient to treat the needs being presented. When we submit documentation for services rendered, we get denials at best and no response at worst. When our fiscal team follows up, they tell us that they did not receive the request or we were missing documentation. When that's proven to be untrue because we documented previous requests, additional excuses come: the claim was made too late, this isn't enough documentation, the service wasn't necessary. The few times we have received payment, itemization of the reimbursement is not included, which affects how we are able to track payments. We continue requesting itemization, but often to no avail. Even now, the State of Illinois owes Saint Anthony Hospital over $20 million in services already rendered.
We believe that the current system payment model utilizing for-profit MCOs supports systemic racism because it continues to keep marginalized communities unhealthy by forcing safety net hospitals like Saint Anthony to face unnecessary fiscal barriers. Unlike other hospitals with a more diverse payor mix, less than 4% of patients at our safety net hospital have private insurance. We are afraid that we will not be able to continue to provide the high quality of care with the current MCO model that works to deny payment. In fact, Saint Anthony Hospital seeks advocacy assistance from larger hospital systems in Illinois that have a better commercial payor mix and depend less on MCO payments.
Saint Anthony Hospital conducts regular community health needs assessments, which provide the hospital valuable information about social determinants of health and play a key role in determining how we structure and provide services. Our most recent community health needs assessment conducted in 2018 determined that care for their children was a substantial community need. Additionally, according to the National Partnership for Women & Families, women of color are more 3 to 4 times more likely than white women to have a pregnancy-related death.4 In an era where so many hospitals are eliminating pediatric units due to high costs to the hospital,5 Saint Anthony Hospital not only chose to continue providing high quality pediatric and obstetric care, but we prioritized budget funds and expanded our services to include critical care pediatric services. We were recognized as a community children's hospital in 2018 by Illinois, and Saint Anthony was the first hospital in Chicago to receive the perinatal care certification from the Joint Commission in 2019.
Our Community Wellness Program is a major component in ensuring that our services continue to fit the needs of the community. The program has been embedded in the surrounding communities for over 20 years. The Community Wellness Program includes health care access, pregnancy testing, case management, mental health counseling and family support. These services are offered at no cost to community members. The program evolved out of the recognition of much-needed mental health services in our primary service area more than 20 years ago. The Community Wellness Department, which now employs 35 people and includes satellite offices in our service areas, extends our reach to serve over 12 communities. Saint Anthony Hospital has used operations to fund this department at a level that has varied between 20% and 30% of the hospital's budget. The hospital's fiscal commitment to the Community Wellness Department continues, even at a time when reimbursement from MCOs for services already rendered is often delayed or denied.
Funding matters when it comes to creating systems to combat systemic racism. However, some recent changes in Illinois policy haven't helped improve health care. In an effort to be "cost effective" under former Illinois Gov. Bruce Rauner in 2017, the state switched to a system where insurance businesses and other organizations bid on contracts to handle the reimbursements to hospitals and providers. The State of Illinois benefits from eliminating its role in administering the program, and the MCOs benefit as they are able to keep a considerable amount of the funding as their administration fee. That is a new cost to the Illinois Medicaid system, which is not supplemented by an increase in funding. Six of the seven businesses selected for these MCO contracts were for-profit companies; when profits are the priority and responsibility to investors the goal, the commitment to quality of care to providers and patients may experience some slippage. For-profit MCOs determine the amount and quality of care a patient receives when they control what services can be provided and the payment for that care. Doctors recommend tests, procedures and care plans based on the needs of the patients in front of them, but the MCOs have the authority to determine if they'll reimburse for the ordered services. It's a simple equation to figure that the more claims denied, the more profits the company can claim.
For FY 2020, the MCOs are projected to keep as administrative profits approximately $2.5 billion of the $16 billion projected to be distributed to them.6 With the pool of money left, the MCOs have exclusive control and decision-making power, with few state regulations, over determining if a claim submitted by a hospital or doctor is necessary and appropriate for reimbursement.7 In fact, when guidelines and protocols exist, they are often not enforced by the state, in our experience. Moreover, when the payment is finally received, the payment provides no information as to what the reimbursement covers. This information is critical, as many facilities like Saint Anthony Hospital are entitled to receive add-on payments to the base claim, given the patients served and services provided. Additionally, the provider tax payment should also be included, but without itemization, we have no way of knowing what the reimbursement covers. Without this clarity, providers have no insight into what payment is being received and whether or not it is correct.
Since the implementation of MCOs in Illinois, Saint Anthony Hospital has been flooded with denials from MCOs because, more often than not, the MCO is determining if a claim is valid for Medicaid populations, which consist mainly of poor people, often people of color. While denials for payment from MCOs impact all Illinois hospital systems interacting with MCOs on some level, larger hospital systems are less vulnerable to the negative financial impact, as they do not serve populations where over 95% of their patients are on Medicare, Medicaid or charity care, as is Saint Anthony.
Larger systems have high levels of privately insured patients and have higher rates of reimbursements. These higher rates not only allow those providers to absorb the negative impacts of the MCO model, but it increases their ability to have the funding to invest in staff and systems to combat the tactics used by the MCOs to deny payments. Saint Anthony Hospital has a payor mix of about 92% Medicare and Medicaid, 4% charity, and less than 4% privately insured patients.
Saint Anthony Hospital is located between two communities in Chicago, allowing us to provide health care to Little Village, a predominantly Mexican American community and North Lawndale, a predominantly African American community. Our reach extends to many other Chicago neighborhoods on the West and Southwest sides, due to partnerships with other organizations. We continue to provide high quality care, but reimbursements continue to lag.
We have committed to, and will continue to do our part, providing high-quality care and a community-centered approach for as long as we can. However, we are at a point now financially where we are asking larger hospital systems, especially larger Catholic health care systems with facilities in Illinois and across the country, to use the resources they receive in serving more affluent communities and advocate on our behalf. As brothers and sisters in Catholic health care, we should be able to call upon one another for support because those we serve need us now more than ever. Pope Francis has denounced what he has called the throwaway society on numerous occasions because it overwhelmingly harms people in the most vulnerable communities — the very communities Saint Anthony Hospital serves.8 We strongly urge those from larger Catholic hospital systems to take a stand against a system set up to make safety net hospitals fail.
EDEN TAKHSH, an obstetrician-gynecologist, is vice president and chief quality officer for Saint Anthony Hospital. JAMES SIFUENTES is the hospital's senior vice president, mission and community development. GENESSA SCHULTZ is the director of community wellness for Saint Anthony Hospital.
NOTES
- Vernillia R. Randall, "Impact of Managed Care Organizations on Ethnic Americans and Underserved Populations," Managed Care and Minorities, Institute on Race, Health Care and the Law, 2008, academic.udayton.edu/health/02organ/manage02.htm.
- Professional Research Consultants, Inc. "2018 Community Health Needs Assessment Report," Foundation and Giving, Saint Anthony Hospital, March 2019, sahchicago.org/images/foundation-and-giving/community-benefits-report/2018-PRC-CHNA-Report-SaintAnthonyHospital.pdf.
- Illinois Health and Hospital Association, "Quality and Safety," 2020, www.team-iha.org/quality-and-safety.
- "Black Women's Maternal Health: A Multifaceted Approach to Addressing Persistent and Dire Health Disparities," National Partnership for Women & Families website, 2018, https://www.nationalpartnership.org/our-work/health/reports/black-womens-maternal-health.html.
- Weijen W. Chang, MD, SFHM, FAAP, "The Rapidly Disappearing Community Pediatric Inpatient Unit," The Hospitalist, July 12, 2018, https://www.the-hospitalist.org/hospitalist/article/170115/pediatrics/rapidly-disappearing-community-pediatric-inpatient-unit.
- Illinois State Comptroller, "Fiscal Year 2020 State Spending on Managed Care Organizations," https://illinoiscomptroller.gov/Office/MCO/.
- Alexia Elejalde-Ruiz, "Audit Slams State Agency That Oversees Medicaid for Inadequately Monitoring $7.11 Billion in Payments," Chicago Tribune, January 24, 2018, https://www.chicagotribune.com/business/ct-biz- medicaid-managed-care-auditor-general-report-0124-story.html.
- Nicole Winfield and Jacobo Garcia, "Pope Denounces 'Throwaway' Culture of Consumer Society," The Associated Press, July 9, 2015, https://www.businessinsider.com/pope-denounces-throwaway-culture-of-consumer-society-2015-7.