BY: JOHN CAPASSO and Sr. MARY PERSICO, IHM, Ed.D.
The Program of All-inclusive Care for the Elderly (PACE) is centered on the belief that it is better for the well-being of seniors with chronic care needs — and their families — to be served in the community whenever possible. First introduced as a benefit in the Balanced Budget Act of 1997, PACE is modeled on an innovative senior care delivery system created in the early 1970s in San Francisco, and later tested through federal demonstration projects in the 1980s.
PACE serves individuals who are age 55 or older, certified by their state to need nursing- home care, able to safely live in their homes and who reside in a PACE service area. The majority of PACE participants are dual eligibles, so Medicaid and Medicare pay a capitated rate for their care. PACE programs use a caregiver team to provide the entire continuum of care and services to seniors with chronic care needs while helping them maintain independence in their homes for as long as possible.
The primary goal of PACE is to keep participants well and out of institutions. Participants benefit because their health is closely monitored to minimize acute episodes, and the state benefits because the cost of community care is far lower than institutional care. If a PACE enrollee does need nursing home or acute care, the PACE program pays for it and continues to coordinate the enrollee's overall care.
The commitment to this much-needed service is substantial. The capital and operating expenses of each program can cost upwards of $5 million before operations achieve a break-even point. Usually, enrollment must reach a level of approximately 125 participants before achieving the financial break-even point, which typically takes 18 to 24 months. The total time from initial planning to breakeven can be as long as five years.
CATHOLIC HEALTH EAST'S PACE PROGRAMS
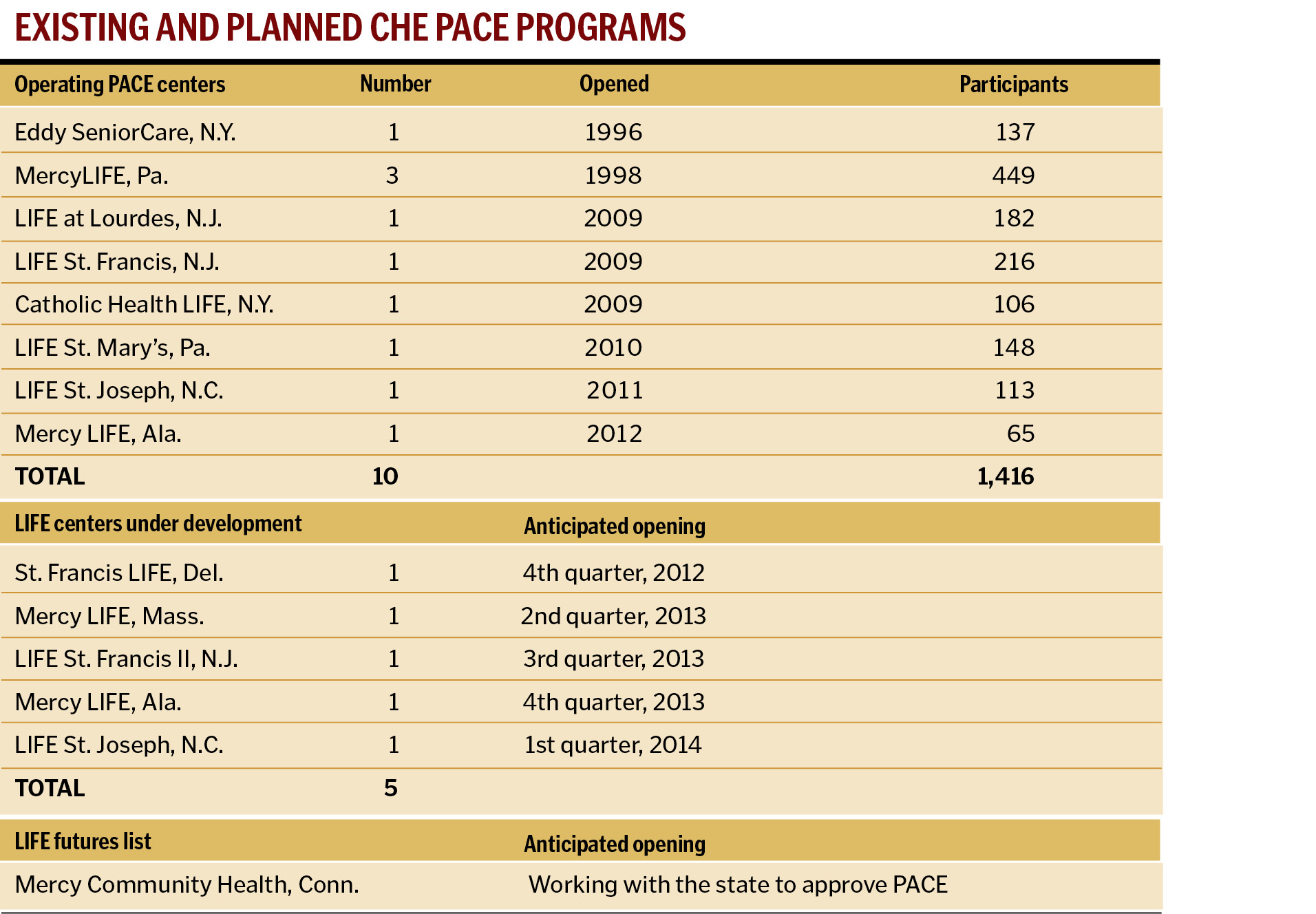
CHE, headquartered in Newtown Square, Pa., owns and operates 10 PACE programs in four states, serving more than 1,400 individuals. Currently the largest operator of PACE programs in the United States, CHE hopes to expand to operate 16 PACE centers in eight states within the next few years.
Since well before the Affordable Care Act (ACA) was legislated, CHE has been enthusiastic about PACE because it serves the poor — one of CHE's core values — through a cohesive program that is financially sustainable. PACE is one of the many ways CHE serves the communities in which its facilities are located.
In 1996, Eddy SeniorCare, Albany, N.Y., (now part of St. Peter's Health Partners) opened one of the first PACE programs in the nation. Mercy Health System of Southeastern Pennsylvania opened its first PACE program, known as Mercy LIFE (Living Independently For Elders), in 1998; this program expanded to three locations over the ensuing years. Currently, they serve approximately 450 participants at the three PACE centers. Both Eddy and Mercy initiated PACE when it was in a demonstration program status. Shortly thereafter, PACE became a federal program funded by Medicare and available across the country.
It wasn't until 2009 that three additional PACE programs were opened by CHE affiliates in New York and New Jersey: Catholic Health System, Buffalo, N.Y.; Lourdes Health System, Camden, N.J.; and St. Francis Medical Center, Trenton, N.J. The New Jersey-based programs reached capacity within two years, and are both engaged in identifying other locations for expansion.
Since 2010, three additional PACE programs opened at CHE facilities in North Carolina, Alabama and Pennsylvania. Five additional programs are anticipated to open over the next 18 months. Provisions in the ACA for expanding Medicaid, beginning in 2014, may benefit PACE programs by affording them a larger target population. Medicaid eligibility, however, is heavily influenced by the individual states, so any possible increase in the numbers of people covered will vary from state to state.
DEALING WITH DUAL ELIGIBLES: A REGULATORY CONCERN
One of the advantages of PACE is its ability to coordinate Medicaid and Medicare benefits, resulting in improved care transitions, more efficient utilization of services and maintaining wellness in this challenged population.
Also, since PACE is a capitated program and the PACE provider accepts full risk for each participant, the programs have the freedom — and the incentive — to spend resources to maintain participant wellness. For example, a PACE team may arrange to install an air conditioner in a participant's home to help avoid dehydration from summer heat, or to construct access ramps at homes to deter falls — prudent measures to help avoid unnecessary hospitalizations.
Prior to the passage of the ACA, the federal government and many states struggled with how best to serve the dual eligibles, individuals who are enrolled in both Medicare and Medicaid. According to the Medicare Payment Advisory Commission (MedPAC) 2012 Report to Congress, "dual eligibles are a vulnerable and costly group. They tend to be poor and report lower health status than other beneficiaries, and cost Medicare about 60 percent more than non-dual eligibles."
MedPAC reported that, in 2010, there were approximately 9.9 million dual-eligible beneficiaries. Within that population, approximately 2.2 million needed assistance with three or more activities of daily living, which in most states would qualify them for a nursing-home admission. Moreover, one million dual eligibles have greater than five clinical conditions — indicative of their need for significant support.
At the same time, navigating the Medicare and Medicaid programs independent of each other is confusing, costly and inefficient. Less than 2 percent of the dual-eligible population is enrolled in an integrated care program that coordinates benefits, according to MedPAC.
According to the National PACE Association, as of January 2012 there were 87 PACE programs with about 25,000 participants operating in 29 states. With millions of dual eligibles across the country, there is the potential to significantly expand PACE services to improve the lives of this population.
Like PACE, Medicaid managed-care and special-needs programs enroll dual eligibles; however, managed-care organizations have not demonstrated the ability to integrate and align the services provided by their networks of providers. At the same time, the ability of PACE to enroll and serve more participants has been constrained by at least three factors: participants have to receive state approval; payment for participants begins only on the first day of each month; and participants often have to change their primary care physician. Addressing some of these issues could increase enrollment to PACE programs nationwide.
Expansion could also occur by integrating adult day or senior centers with PACE. All PACE centers have occupancy limitations. Currently, when a PACE center reaches its capacity, the only way to increase participants is by developing additional space; this approach is capital intensive and constrains growth. The ability to enroll participants who could utilize adult day or senior centers for the social component of service, while using the PACE center for medical and clinical care, could be an expansion tactic. Using the PACE center as the hub, while using the adult day and senior centers as the spokes, could make PACE available to more people in need.
"PACE growth and expansion throughout the country has the real potential to address cost concerns and improve patient outcomes for the most frail elderly, given the rather unique and intimate nature of the interdisciplinary team and their personal relationship with the participants and families we serve," said Jake Bell, president and CEO, Mercy Medical, Daphne, Ala. "It's one of the few programs where the incentive to provide quality care has a direct impact on the financial performance of the organization. In that respect it is a win/win for both providers and the people served."
CONSISTENCY WITH CHE'S MISSION, VISION AND CORE VALUES
In 1998, when the founders of CHE envisioned a mission that would provide a full range of services to "support healthy communities, including quality medical care and holistic approaches to healing body, spirit and mind," PACE programs were just beginning to make inroads into the health care culture. Nearly 15 years later, their vision has been realized in programs and services throughout the ministry.
The enthusiasm of social workers, therapists, nurses, dietitians, personal care attendants and others whose ministry finds them in a PACE site often is matched by the delight of the women and men who enjoy the benefits of the integrated care they receive. In assuring that the comprehensive medical, social and psychosocial needs of each participant are met, the focus of the interdisciplinary PACE team is clearly person-centered. When they return home from PACE in the evening, many elders find themselves energized by the activities of the day and the opportunities to share memories, stories and to make new friends.
At the Mercy LIFE, Philadelphia, center, a family member recently said, "Mercy LIFE gave my dad a reason to get up in the morning, and the care that he received from the staff kept him going physically, spiritually and emotionally. He looked forward to coming each day and always had a story or two to tell us when he came home."
While the seeds of PACE were first sown in California nearly 40 years ago, regulatory and reimbursement challenges restrained the growth of this innovative care model for many years. The last decade has seen steady growth, with over 80 programs involving tens of thousands of participants nationwide.
PACE is innovative in the way it integrates Medicare and Medicaid, providing coordinated care through a person-centered, holistic model to some of society's most vulnerable individuals. However, if PACE is going to remain a viable care delivery model, it will need to advocate for policy, regulatory and funding solutions to overcome some of the barriers that have prevented its expansion and replication. One such solution, for example, would be to allow programs the flexibility to innovate and test new service delivery models; another would be to allow PACE to expand care to new populations.
For PACE providers, a major area of concern centers on how states are seeking to reform their Medicaid programs, especially those states that have proposed passively enrolling individuals in Medicaid managed-care plans, thereby locking the individuals in for a set period of time before they are allowed to self-select out of the plan. CHE believes it is important for individuals to be afforded a choice of health care plans at the front end, which means consumers must receive unbiased education about all their care options, including PACE.
As the baby boomer generation continues to age, the number of people who could benefit from PACE increases dramatically. It behooves our nation to continually look for ways to make PACE programs increasingly available to the needy elderly and their caregivers.
JOHN CAPASSO is president and CEO, Continuing Care Management Services Network, Catholic Health East, Newtown Square, Pa.
Sr. MARY PERSICO, IHM is executive vice president, mission integration, Catholic Health East, Newtown Square, Pa.
KELLY HOPKINS, vice president, home and community services, Continuing Care Management Services Network; KENNETH A. BECKER, vice president, advocacy, government relations and fund development; and SCOTT H. SHARE, vice president, communications; also contributed to this article.
CARE AND SERVICES PROVIDED BY PACE PROGRAMS
- Adult day care that offers nursing; physical, occupational and recreational therapies; social work and personal care
- Medical care provided by a PACE physician familiar with the history, needs and preferences of each participant
- Home health care and personal care
- Prescription drugs
- Meals and nutritional counseling
- Social services
- Medical specialists in such fields as audiology, dentistry, optometry, podiatry and speech therapy
- Respite care
- Hospital and nursing-home care when necessary
ONE FAMILY'S PACE STORY
Joanne's elderly mother, Irene, was living alone in a Pittsburgh-area apartment. Despite her advanced age, she was active in the community, a regular churchgoer, with many friends. Then one day she suffered a stroke, and her life changed forever.
"A girl found me on the floor of my apartment," said Irene. "I don't know how long I had been laying there. They called the ambulance and it took me to the hospital. After that, Joanne was after me to come live with her. I was scared to be in that apartment by myself."
"It became difficult for her to be alone, and there were no family members nearby," said Joanne. "My mom needed to be with family who could help care for her. So we made the decision that she would come to New Jersey to live with me."
"Mom had lived in the same town her entire life. She was living a few blocks from where she was born," said Joanne. "She was about to turn 87 years old. She had to leave her church, her friends, all of her social activities … and move to a place where I am the only one she knows. She was very isolated."
"I was active in different organizations; I was president of two of them," said Irene. "I was a busy woman. Now I go to church and I can't even say hello to anyone … I don't know a soul there. It's a different life."
"I was searching online for a PACE program in New Jersey… and I found the LIFE at Lourdes program" said Joanne. "We called, and they had us come over. We met the staff and toured the facility. We both liked it. Mom was one of the first participants when the new facility opened. The program gave her the opportunity to be with other people two days a week. It gave her the chance to make new friends and have that social outlet … it was very important to her because she is a very social person."
"Mom goes to the LIFE at Lourdes program two days a week," said Joanne. "She has breakfast and lunch there. They pick her up in the morning, and they drop her off in the afternoon. So that gives me the time to do the work that I need to do."
"Joanne needs a little time for herself," said Irene. "When I'm at LIFE at Lourdes, she can go do the stuff that she needs to do, and she knows I'm being taken care of."
"I just can't say enough good things about the program," said Joanne. "They're very caring, they're very loving, they're very concerned. Everyone is always pleasant. They love her and appreciate her. They value her. I know she's in good hands when she's there."
"I love it," said Irene. "It's a very, very nice organization. I enjoy it … I really do!"
Copyright © 2012 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.