BY: MARC BARD, MD; PAUL CONLON, Pharm.D., JD; GALE GARTNER; and P. TERRENCE O'ROURKE, MD
Dr. Conlon is senior vice president, clinical operations improvement; Ms. Gartner is director, physician services; and Dr. O'Rourke is executive vice president and chief medical officer; all at Trinity Health, Novi, Mich. Dr. Bard is president and CEO, The Bard Group, Needham, Mass.
In life, relationships are tricky things. If the chemistry is good, you have the makings of a beautiful and rewarding partnership. Bad chemistry produces hard feelings and dysfunction. The catalyst for chemistry is trust, or lack thereof.
The same applies to relationships between hospital administrators and physicians. A hospital's financial success and clinical reputation stems largely from its medical staff. The ability to recruit, retain and build physician loyalty is critical to the hospital's reputation and market position, and, ultimately, to its ability to sustain a healing ministry.
Physicians rely on hospitals to provide them with tools, facilities and caregivers to achieve superb clinical outcomes. They look for secure and predictable income arrangements, input into strategic leadership decisions, a highly efficient and collegial working environment and, above all, the opportunity to provide the best care possible for their patients. Also, many physicians value quality of life and stability in their communities, tightly linking them to the reputation of "their hospital."1
At first glance, the wants and needs of physicians and administrators may appear to be mutually beneficial. Yet, industry pressures often lead to dissonance and conflict. Physicians face the pressures of declining compensation, misaligned incentives to provide excellent care, and difficult malpractice environments in many markets. They want hospitals to help lessen the burden of these market forces. They also need help addressing concerns related to consumerism, science and technology, chronic diseases, and costs. Turf battles, time demands, information overload and lifestyle desires threaten the quality of their personal and professional lives.
Meanwhile, hospitals are pushing for greater physician integration as a defensive measure to protect market share and volumes. Key clinical service lines, especially surgery, imaging and other outpatient services, continue to be at risk of loss to niche providers, many with physician investors.2 Hospital leaders are sleepless over call coverage, increasingly complex physician relationships, specialization and communication, information technology issues, competition and unrelenting capital needs.
With such an array of challenges, a long-term commitment by both parties is needed to create a highly aligned and successful health care delivery system. Physician partnership and alignment with management are integral to this goal.
Mission Critical
In 2007, Trinity Health — a system that collaborates with more than 13,000 practicing physicians in 44 community hospitals — embarked on a journey to strengthen the hospital-physician partnership. As early research and discussion unfolded, Trinity Health leaders reached an overarching conclusion: Sustainable success and growth is critically dependent on establishing a common aim and vision with physicians.
In creating a vision for the partnership, we looked to the mission of Trinity Health:
"We serve together in the spirit of the Gospel to heal body, mind and spirit, to improve the health of our communities and to steward the resources entrusted to us."
With mission fulfillment as the underpinning goal, administrators of Trinity Health worked in partnership with physician leaders to outline the parameters of a new physician alignment strategy. The following definition of physician alignment by The Bard Group, a national health care consulting firm, summarizes the direction of the work:
"Physician alignment is the degree to which physicians and hospitals, acting out of enlightened self-interest, operate inside a common vision and set of goals and the acknowledgment of a shared destiny."
The words "shared destiny" resonated with physician leaders and liaisons. Trinity Health is grounded in meeting the needs of patients across the care continuum. In the words of the health system's mission statement, "we serve together to improve the health of our communities."
The Evolution of Alignment
As health system leaders ventured forward, no shortage of ideas and strategies to review existed. Many were complex and confusing. Some were discarded because of regulatory concerns. Others contradicted the system's Catholic identity. As a faith-based, national health organization of teaching hospitals, medical centers and community hospitals serving diverse communities in seven states, leaders discovered wide variation in current approaches and degrees of success.
Leaders organized alignment models under distinct categories. Through the years, hospital-physician relationships have been assigned various terms reflecting the thinking of the day. Occasionally, these terms are used interchangeably, but the belief is that the following three models are different initiatives:
1) Physician Integration
This model evolved in response to the inefficiency found in many physician practices that hospital administrators purchased in the late 1990s. Under this model, hospital system leaders employ their physicians or sponsor their own physician groups. But integrating physician practices into the hospital's culture and operations can be more complex and difficult than expected. While some find success, many hospital administrators eventually divest their ownership of physicians' practices.
2) Physician Engagement
A popular trend at the start of the millennium, this model is based on the concept of attraction. Dominated by joint ventures such as a co-owned ambulatory surgical centers, and based primarily on financial gain, these partnerships often fall apart if one or both parties decide to pursue more attractive ventures.
3) Physician Alignment
This relationship-based model involves hospitals and physicians working collaboratively toward a common vision. Both parties share the risk, governance and reward. The model has had encouraging results in the creation of sustainable partnerships.
Five Dimensions of Alignment
Any physician-hospital arrangement aimed at alignment can be filtered through the following five dimensions, which help to define objectives:
1) Behavioral Alignment
Actions that support a facility's clinical, service and business goals and are characterized by behaviors that reflect collegiality among caregivers. They include being accessible and responsive, treating all staff members with respect, and remaining open to new ideas.
2) Performance Alignment
Actions that support targets related to growth and productivity; compliance with quality and safety standards; adherence to established programs, protocols and standards of care; and managing referrals within the system.
3) Operational Alignment
Actions that support goals related to efficiency, such as timely arrival and turnaround in the operating room, responsiveness to emergency department consultations, management of length of stays, and development of effective physician leaders into physician manager positions and directorships.
4) Strategic Alignment
Actions that position both the hospital and physicians for long-term growth and viability, such as participation in service lines and centers of excellence, relocating services for strategic value, and supporting non-self-serving investments for the hospital.
5) Economic Alignment
Actions that support global contracts, joint ventures, pay for performance initiatives; ethical gain sharing, co-management contract expectations, employment, and other economic relationships.
Since each institution's relationship between its physicians and administrators is different, Trinity Health leaders use these five dimensions as a prism in its various arrangements aimed at physician alignment. Some arrangements place greater emphasis on one dimension over others. As an example, some co-owned ambulatory surgical centers emphasize economic alignment and less attention is given to behavioral, operational or strategic alignment.
A model that can strike the right balance with all five dimensions has the greatest potential for long-term success and mission fulfillment. Above all else, the partnership requires trust and a shared vision.
Beyond Economics
The more elements are aligned, the better and more durable the outcome. Think of the elements as gears in a machine. If they all mesh, the machine works optimally. Can pure economic alignment work? Yes, for a while, but it won't have the sustainability, flexibility and adaptability that a complete alignment would. Its continued success will always be threatened by changing circumstances in the environment.
Believe it or not, the business end of a physician alignment model is the easy part. Achieving mutual support and partnership is a much more deliberate and intentional process that goes way beyond the signing of a contract.
How is true alignment produced in today's fractured environment? The primary focus must begin with the physicians' identified community of practice. From this vantage point, leaders should consider the following five steps:
- State initial intentions and rationale clearly and honestly
- Organize the physicians in ways that encourage interdependence around shared services such as information technology initiatives, protocol development and service-line management
- Empower hospital leadership to build relationships with physicians and hold them accountable for maintaining open communication and shared decision-making
- Engage physicians as collaborators in a shared destiny
- Start at the beginning with a culture of full transparency
Trusted Health Partner
Again, the bedrock of any successful physician alignment strategy is the ability to build trust between physicians and hospital leaders, one relationship at a time. Trust, the essential ingredient to collaboration and open communication, takes years to develop. For communication to work well, both hospitals and physicians must have a relationship based on mutual respect, a sense of value, and a personal investment in the improvement of care. Careful attention and intention to the values of transparency, honesty and commitment must be imbedded in strategies aimed at physician alignment.
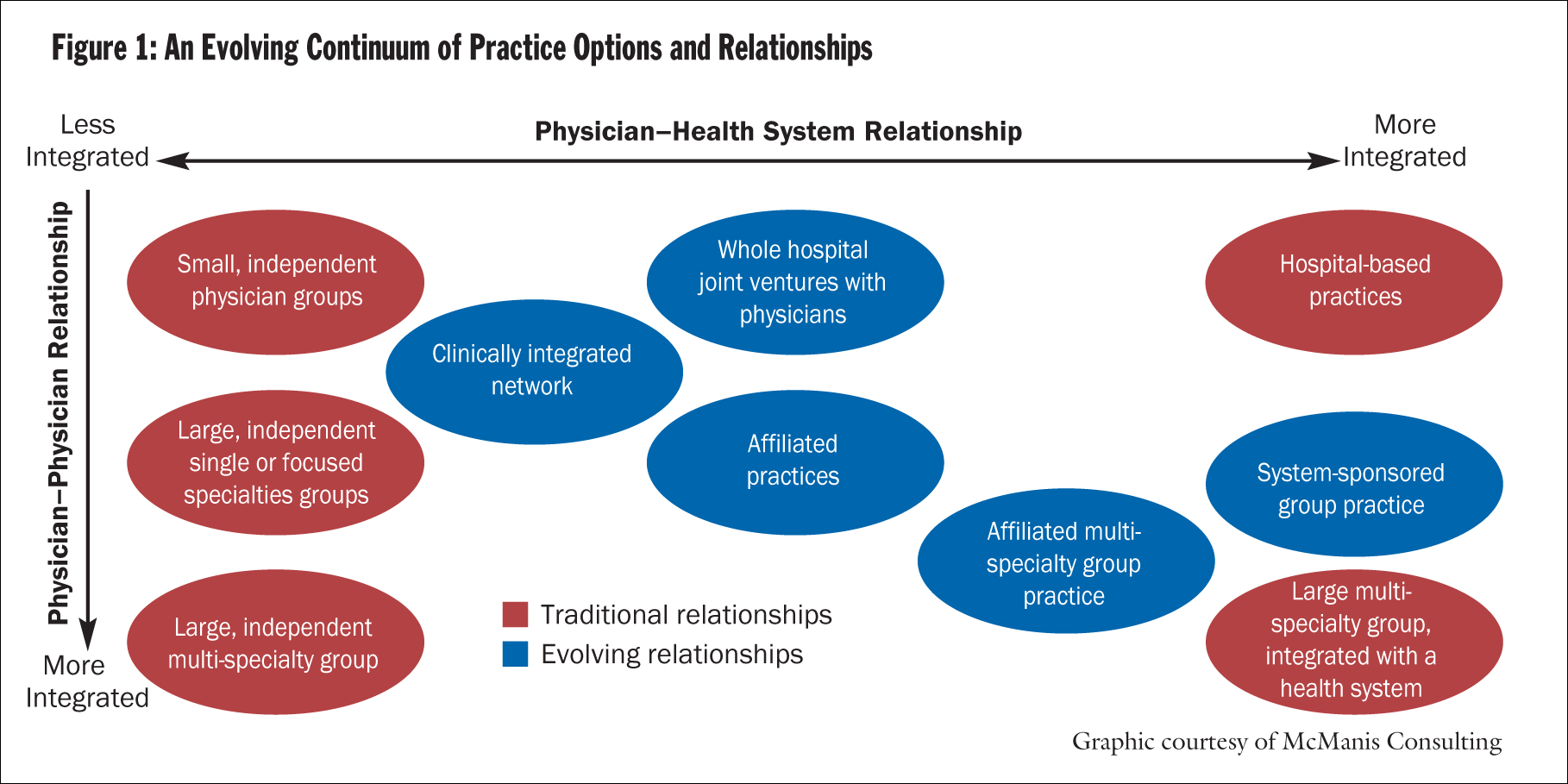
A revealing statement in a white paper entitled Physician Relations and Clinical Integration3 summarizes this theme: "The steps in developing durable relationships — relationships that adjust to changing circumstances over time — are to listen, then to dialogue, then to model possible options, then to listen and dialogue again." (Figure 1.)
But no matter how strong a partnership becomes, it is most vulnerable when management changes occur. Although it's common to see a physician stay on staff for decades, the average tenure of a CEO is just four years. Many seasoned physicians can tell war stories about former administrations that have destroyed their trust in the system. Some bear emotional scars that have left them jaded toward incoming executive management teams. When strategic initiatives shift with each leadership change, it becomes increasingly more difficult to win their support.
During these periods of change and transition, it is important to reinforce the partnership's shared mission and vision. Through effective communication and a steadfast commitment to building trust, both physicians and hospital leaders can rise above differences in the best interest of the one person who is counting on us to work together — the patient.
NOTES
- Andis Robeznieks, "Hot Commodity: Survey Shows Doc Pay Keeps Climbing, but Raises Moderating," Modern Healthcare 38 (July 14, 2008): 26.
- Lisa Goldstein, "Not-for-Profit Hospital-Physician Integration: New Strategies or Back to the Future?", Moody's Special Comment (September 2005): 3. Reprints available for purchase at (212) 553-1658 or www.moodys.com.
- Keith Moore and Dean Coddington, Physician Relations and Clinical Integration (Denver: McManis Consulting, 2008), 13. The document is available by contacting McManis Consulting at (202) 661-2171.
The Making of an Effective Alignment: Saint Mary's and Advantage Health
For more than 25 years, Saint Mary's Health Care, a hospital in the Trinity Health system, and its primary care group, Advantage Health Physicians Network, have been partners in serving the health needs of the people of Grand Rapids, Mich.
In the early days of their joint venture arrangement, hospital and physician leaders created a culture of "authentic shared decision-making," manifested by a single-minded focus on improvement through good times and bad. With physicians and hospital leaders sharing every aspect of management and strategic planning, Saint Mary's has cultivated a strong referral network, built-in recruitment, loyal patients and a mix of vital patient-centered services.
Today, with more than 120 primary care physicians and specialists in 18 offices, Advantage Health represents the majority of Saint Mary's volume of 19,500 annual admissions.
"Advantage has become such an integral part of Saint Mary's, we wouldn't think of adding a new service unless we first speak to them," said Phil McCorkle, president and chief executive officer, Saint Mary's Health Care.
David Blair, MD, president and CEO of Advantage, lists the following six key attributes of the successful hospital-physician alignment model at Saint Mary's.
1) Believe in the Mission
Saint Mary's and its parent company, Trinity Health, have a mission to "heal body, mind and spirit" and "improve the health of our communities," especially to the underserved. Physicians in the network appreciate the attention to the "relationship side of care," Blair said.
"We encourage our patients to be active in their care, as if they were a member of our family."
2) Share Decision-Making
Saint Mary's Health Care may own the assets of Advantage Health Physicians Network, but the governance board is a 50-50 split between Saint Mary's leaders and the physicians. "That is the real secret to our model - physicians are highly involved in every aspect of planning, operations and growth," Blair said. It has been noted that the shared decision-making has become so strong that it is difficult to distinguish where the hospital input ends and the physician input begins.
Working together, Saint Mary's has built the Lacks Cancer Center and Hauenstein Neuroscience Center and opened Saint Mary's Southwest, an 86,000-square-foot outpatient center providing a wide range of services, and implemented computerized health records and a physician order entry system. Blair said the transition from paper to digital records was not easy, but physician involvement in the system's design and implementation has led to an 85 percent usage rate among active practitioners.
3) Trust One Another
Over the years, the hospital-physician partnership has experienced several strategic shifts and leadership changes. Within a collaborative board structure, management styles and personalities are important to the partnership's success. The relationship has become "very deep and sophisticated," Blair said. "There is a strong sense of mutuality."
4) Steward the Resources
One physician summed up the challenges in the marketplace as a perfect storm of declining medical school enrollment, retiring physicians, declining reimbursements, a weakening economy, and an aging population with increased need for health care.
With external forces threatening to erode work-life balance and revenue streams, Saint Mary's and the Advantage network's officials focus on management efficiency and cost savings.
"We work very hard to build financial models and business plans to ensure long-term viability and stable incomes," Blair said. Last year, Advantage opened four new offices and added 40 new physicians to its network.
5) Allow Freedom to Serve
The alignment model allows Advantage physician leaders to explore better solutions to the current primary care system. One approach to chronic disease management is a patient-centered "medical home" program, in which the doctor follows up office visits with phone calls and e-mails to ensure that patients take their prescriptions and stay healthy. Advocates say the approach should help contain costs and improve the health of people with diabetes and other chronic diseases. A medical home could also lead to fewer specialty referrals, hospital admissions and unnecessary tests and procedures. The idea is to close the gaps in chronic disease care, lessen the time required to reach primary care doctors, and improve outcomes for patients.
"A lot of physician groups are stuck in the trenches fighting fires," Blair said. "We have the ability to think about tomorrow's work and how we can improve primary care."
6) Never Rest on Laurels
Under the leadership of the hospital's chief of staff, aligned physicians have begun redesigning their relationships to one another and to Saint Mary's. Included in the work was the formation of new physician councils giving physicians more opportunities to express opinions; a physician survey; consultant-guided work on topics such as new models of medical staff/hospital relationships; and a study of physician supply and demand in the Grand Rapids service area.
Result: Service Excellence
Saint Mary's Health Care has become a high performing network of top-quality primary care physicians and specialists serving a wide array of health needs in state-of-the-art facilities. Both physician and patient satisfaction scores are above the national mean. Advantage doctors have received the Michigan Governor's Award for Excellence five years in a row. Blue Care Network has recognized the network for achieving the highest quality health care in western Michigan.
Further, 57 Advantage physicians were among the 175 physicians receiving the National Commission for Quality Assurance's award for Outstanding Care of Diabetes in Michigan.
Through the years, several founding physician leaders at Advantage have advanced to leadership roles within Trinity Health, including Bruce Van Cleave, MD, who served as Trinity Health's executive vice president and chief medical officer for 13 years, and two who have led medical staffs at other system hospitals.
"We have done very well together," Blair said. "And we are excited to find more ways to strengthen our relationship."
Doug Edema, MD, a former head of the network, is now the vice president and chief operating officer at St. Joseph Mercy Livingston Hospital. He credits attention to relationships for the partnership's success. "It's not about any business model that makes it successful," he said. "It's a continual process of listening to and understanding each other's needs that makes it so strong."
Copyright © 2008 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.