BY: BENJAMIN F. MILLER, PsyD
Illustration by Roy Scott
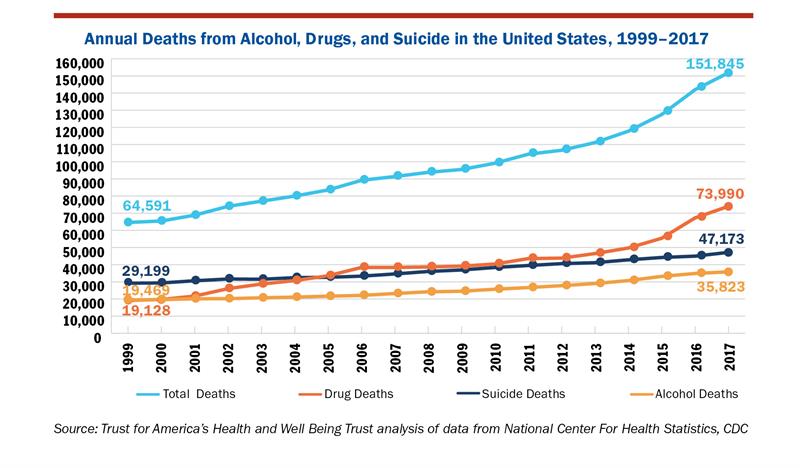
The data is going in the wrong direction. While life expectancy has been on the rise since the 1960s, its sharp decline over the last three years is a sign that something is fundamentally broken in the United States.1 It's 2020, and we are losing more lives to preventable causes than ever before. Deaths due to drugs, alcohol and suicide are at an all-time high, and our country is hurting in ways that are multifaceted — attributable to overlapping issues and circumstances. For some, it may be access to affordable health care. For others, it may have more to do with social and economic factors.2 Loneliness, worry, isolation and issues of belonging are key drivers of despair, and we must be bold in our vision and courageous in our decision making if we are serious about making a difference in our country's health.3
For more than a decade, the dominant health policy landscape has focused on improving outcomes, decreasing cost and enhancing the patient experience.4 And while these goals are important, health policy strategy has often treated mental health as an afterthought. Although there have been many well-meaning but disconnected attempts to integrate, we have yet to see a robust policy agenda that centers on mental health. Our country has a mental health problem, and the solutions have been as fragmented as the systems we have created to address it. Faced with unprecedented urgency, it is time to bring mental health to the top of our agenda.
This article describes a way forward — a specific policy framework and options to consider if we are serious about doing something different for mental health. Beginning with a brief history, flowing into possible solutions and closing with a framework and policy call to action, this article will attempt to be a primer for mental health policy.
HOW WE GOT HERE
While the history of mental health has been documented extensively elsewhere,5 at a high level one could describe the United States as having gone through several phases of mental health reform, with the most current one being the need to treat mental health in our communities.
This current reform dates to 1963. President John F. Kennedy made the momentous decision to deinstitutionalize mental health, which was seen by many as a positive step in the right direction. The inhumane and often brutal treatment of those with mental illness served as examples of misunderstanding mental health and failing the people who needed help the most. President Kennedy described the 1963 law:
"This approach relies primarily upon the new knowledge and new drugs acquired and developed in recent years which make it possible for the most mentally ill to be successfully and quickly treated in their communities and returned to a useful place in society."6
A multitude of policies, all intended to support this new approach, have been instituted and codified. The emergence of a separate system for mental health had officially been created, which meant that new financing and delivery models, health insurance benefits and other related factors were also new and in need of policy to support them. These critical first steps of the third mental health reform were essential in establishing a new system of care — and yet in 2020, while scientific knowledge and mental health policies have advanced, President Kennedy's vision remains aspirational.
People still have to wait too long to get access to mental health care, and stigma — both social and structural — remains a barrier to addressing mental health issues. While well-intentioned, clinical and programmatic fragmentation have had unintended consequences, including the creation of an entirely separate system of care that is often disconnected from the rest of health care. In addition, community mental health centers, an entirely sound idea, were never given adequate resources to develop the capacity needed to meet the needs for mental health treatment.
A REVOLUTION IN INTEGRATION
If a culture of fragmentation is the dominant problem for addressing mental health, then integration must be the solution. Many have touted the benefits of more integrated programs, and the evidence is robust about its impact.7 However, like many good ideas in health care, without systemic implementation, even the most effective programs run the risk of failing or, even worse, not being scaled and sustained despite initial success.
Integrating mental health and primary care provides one of the best-use cases for successfully integrating mental health into a medical team approach. The Agency for Healthcare Research and Quality defines this as: "The care that results from a practice team of primary care and behavioral health clinicians, working together with patients and families, using a systematic and cost-effective approach to provide patient-centered care for a defined population. This care may address mental health and substance abuse conditions, health behaviors (including their contribution to chronic medical illnesses), life stressors and crises, stress-related physical symptoms, and ineffective patterns of health care utilization."8
At a health system level, there are multiple opportunities to apply an integration lens to more traditional medical care. Consider some of the elements from the lexicon: a team approach to care that is rooted in the full continuum of how patients and their families present with mental health needs. Because of the pervasiveness of mental health across all health conditions, it is likely that patients' clinical outcomes and overall experience will be enhanced because they had access to another expert who could help them with their mental health.
However, like so many good ideas on mental health and integration, sustaining these models is challenging in part because of the historical roots of how we pay for mental health care (separate), and the policies that limit how well we integrate. This is a propitious moment to do something about mental health in this country, and policy is one meaningful mechanism to help address this crisis.
EVERYONE HAS A ROLE IN POLICY
Recently, Well Being Trust, in partnership with several key collaborators, launched a federal policy guide entitled "Healing the Nation: Advancing Mental Health and Addiction Policy." The title tells a bit about the story: People are hurting, and policies should be responsive to the pervasive mental health needs that are being unmet. The goal is to provide members of Congress a comprehensive guide on ways to impact mental health through policy. Leveraging a framework for action, "Healing the Nation" offers a plan that will start with the federal government and extend into our states and communities.
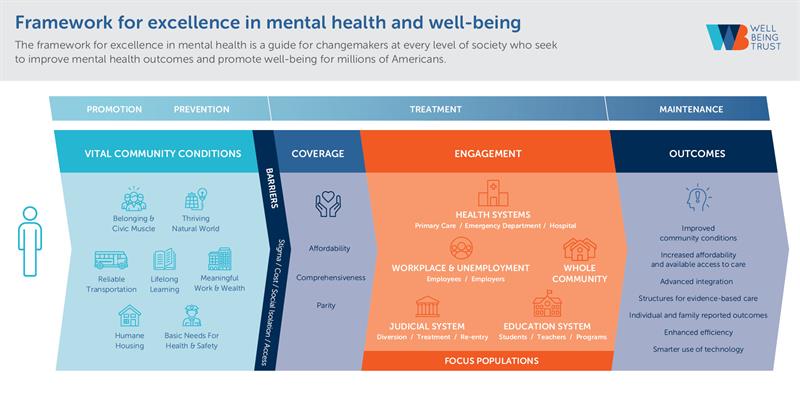 The framework within "Healing the Nation" focuses on multiple angles for engagement with a specific emphasis on five main entry points for policy: health systems; judicial systems; education systems; workplace and unemployment; and the whole community. The framework also highlights populations that have been impacted differently by the mental health and addiction crisis. The end goal of the policy guide and framework is to offer a more integrated approach that could bring mental health into all our health policies.
The framework within "Healing the Nation" focuses on multiple angles for engagement with a specific emphasis on five main entry points for policy: health systems; judicial systems; education systems; workplace and unemployment; and the whole community. The framework also highlights populations that have been impacted differently by the mental health and addiction crisis. The end goal of the policy guide and framework is to offer a more integrated approach that could bring mental health into all our health policies.
Below are some examples of the types of health system policies in "Healing the Nation." All policies as well as the framework can be found at http://healingthenation.wellbeingtrust.org/
- The federal government should ensure that hospital payment models and quality programs incentivize assessing mental health at every interaction as a vital sign, and not only during well visits. This should include integrating screening and treatment into episode-based payment models for health conditions that often are diagnosed and treated simultaneously with mental health conditions, such as cardiovascular diseases, cancers and pulmonary diseases.
- Suicide and mental health crises should be included as part of hospital safety initiatives, and evidence-based strategies should be integrated into federally funded hospital quality improvement programs. Examples include Zero Suicide, a program that helps health systems embed systems to identify and treat individuals at risk for suicide.
- The federal government should invest in piloting and scaling innovative information technology solutions to improve the successful triage and coordination of care for individuals with mental health conditions that present to emergency medical services or the emergency department, including connections with social services.
- The federal government should fund the development and dissemination of evidence-based training and continuing education materials on mental health for emergency department staff.
- And in critical ambulatory care settings, such as primary care:
- The federal government should require that all primary care payment models initiated by the Centers for Medicare and Medicaid Services or by the states through waivers include consideration of whether the model would equip the participating practices with the resources they need to provide integrated mental health care. This should include auditing and revising existing models or initiating new ones and may include carving certain mental health services out of the cost benchmark to ensure that there are adequate incentives for building out integrated care.
- The federal government should mandate prioritization of mental health screening and outcome measures in federal value-based payment models and ensure that the measures are weighted to reflect their importance for population health. Congress should also create a fund that can help low-performing systems improve by implementing evidence-based integration approaches.
- Additional policies should support our workforce:
- The federal government should provide incentives, through graduate medical education, graduate nursing education and other programs for institutions that educate health care professionals to offer training in integrated mental health care.
- Providers should be incentivized to take additional continuing medical education classes on current best practices.9
- Federally funded quality improvement organizations should focus resources on mental health integration across diverse primary care practices and for serving diverse populations, and finance additional learning collaboratives as necessary.
Though not exhaustive, these lists give a sense of the health system solutions within "Healing the Nation." The document delves into specific solutions within the workplace, educational and judicial systems, and for especially impacted populations like youth, LGBTQ+, African Americans, Native Americans and those with co-occurring conditions.
THE TIME FOR REFORM IS NOW
Without seamlessly integrating mental health across our health systems, we are failing people, families, their communities, and ourselves, and policies should reinforce this integrated model of care. With so much focus on health care in politics, it's a shame that so little centers on mental health. While some presidential candidates have brought forth policies that could be transformative for mental health, most debates leave the topic out altogether. Isn't it time for mental health to be on the agenda of every administrator, every elected (and running) official and every stakeholder, including each of us as patients and family members? The rallying cry for the next generation will be integration, so let's begin to do what's right for all of us now.
BENJAMIN F. MILLER is chief strategy officer, Well Being Trust, a national foundation committed to advancing the mental, social and spiritual health of the nation. He lives in Denver.
NOTES
- Steven H. Woolf and Heidi Schoomaker, "Life Expectancy and Mortality Rates in the United States, 1959-2017," JAMA 322, no. 20 (2019): 1996–2016, https://doi.org/10.1001/jama.2019.16932.
- "Pain in the Nation" report, Well Being Trust, Trust for America's Health, http://www.paininthenation.org/assets/pdfs/TFAH-2017-PainNationRpt.pdf.
- Carol Graham and Sergio Pinto, "The Geography of Desperation in America: Labor Force Participation, Mobility Trends, Place, and Well-Being," Brookings website, October 15, 2019, https://www.brookings.edu/research/the-geography-of-desperation-in-america-labor-force-participation-mobility-trends-place-and-well-being/.
- Donald M. Berwick, Thomas W. Nolan and John Whittington, "The Triple Aim: Care, Health, and Cost," Health Affairs 27, no. 3 (2008): 759-69.
- Benjamin F. Miller and Samuel H. Hubley, "The History of Fragmentation and the Promise of Integration" in Handbook of Psychological Assessment in Primary Care Settings, ed. Mark Maruish (New York: Routledge, 2017), 55-73.
- Journal of the Senate of the United States of America, Eighty-eighth Congress, First session beginning January 9, 1963.
- "Integrated Care," National Institute of Mental Health, https://www.nimh.nih.gov/health/topics/integrated-care/index.shtml.
- Charles J. Peek et al., "Lexicon for Behavioral Health and Primary Care Integration: Concepts and Definitions Developed by Expert Consensus," AHRQ Publication No.13-IP001-EF, (Rockville, Md: Agency for Healthcare Research, 2013), accessed January 16, 2020, https://integrationacademy.ahrq.gov/sites/default/files/Lexicon.pdf.
- "Navigating the New Frontier of Mental Health and Addiction: A Guide for the 115th Congress," The Kennedy Forum, https://thekennedyforum-dot-org.s3.amazonaws.com/documents/9/attachments/The_New_Frontier_CongressGuide.pdf?1485267841.
______________
QUESTIONS FOR DISCUSSION
Benjamin Miller is chief strategy officer for Well Being Trust, a national foundation committed to advancing the mental, social and spiritual health of the nation. He is concerned that we are losing more lives to preventable causes — such as addiction and suicide — than ever before. Given what he identifies as the fragmented approach to mental health, he is convinced the solution is in integration: standardizing practice, bridging the silos of health care specialties, funding and insuring mental health on a par with other medical conditions, reducing stigma and social isolation and coordinating efforts for mental health policy.
- Do you experience topics of mental health as a secondary stepchild within health care overall? Can you give examples of how a patient who presents primarily with a physical medical condition might be treated differently than one who presents primarily with a mental health condition?
- Our foundations in Catholic social teaching direct us to uphold the dignity of the whole person. How does your hospital or health system screen for overall health — physical, mental, social, spiritual — in assessing a patient's well-being? Do you think the right questions are being asked? Do you think the right people are asking them? Are your community benefit dollars addressing disparities of care? Do you think you are maximizing a team approach for patient-centered care?
- Miller thinks the time is right for bold action on mental health policy and identifies the five main entry points to move on policy as health systems, judicial systems, education systems, workplace and unemployment, and the broader community. Do you think your health system is primed for such an initiative? Are the right partnerships in place and highly operable? What might your leaders, advocacy experts and mission leaders need to move forward?