BY: RACHEL C. TANNER, MJur
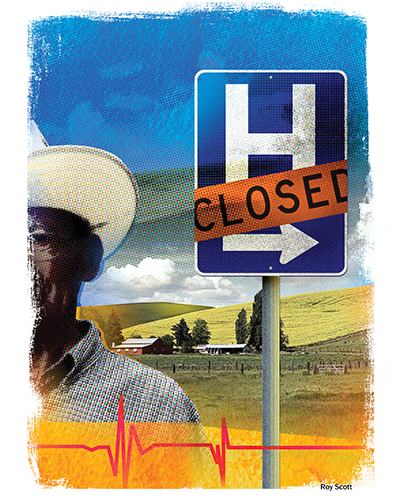
Illustration by Roy Scott
Across the United States, rural communities are facing enormous pressure to survive.Younger generations are leaving to find economic opportunity elsewhere, employers are shutting down, the remaining population is aging, and health care providers and facilities are stretched nearly to the breaking point. In fact, more than 160 rural hospitals have closed since 2005, and 21% of all rural hospitals are at high risk of closure due to financial instability.
One question must follow: if rural communities are facing such difficult challenges, how can Catholic health care leaders help? The answer may lie in public policy. While rural communities face serious policy hurdles, such as workforce sustainability, a challenging payer mix or overly burdensome regulations, we may be able to impact change through advocacy. By contacting our federal elected officials, federal regulators and state leaders, people both in and out of rural America can fight for changes that will shore up rural health care.
WHY RURAL MATTERS
You may be asking yourself why the plight of rural health care is important to people who live in urban or suburban areas. If we set aside the financial implications of closing hospitals, including the overall economic impact to the community, we recognize that the need for care does not go away, but simply shifts to urban and suburban facilities. We must embrace our mission and recognize that people living in rural communities are as much our brothers and sisters as anyone else living on this planet. They often do not have the number of voices needed to advocate for important policy changes, but we can bolster them with the influence of broader health care ministry.
Indeed, many of the founding congregations of Catholic health systems started in rural areas. The women religious looked across our country and saw a need for education, housing, child services and health care. They went where they were needed, regardless of the hardship or economic opportunity. As leaders in Catholic health care, we have a chance to continue that vision and advocate for public policies that serve the vulnerable people and communities found in rural America.
STATE OF RURAL HEALTH CARE
The challenge is daunting. As individuals move away from rural areas to more economically viable cities and suburbs, rural hospitals and health providers are becoming less financially stable and more at risk of closure. Politico reports that since 2005, 162 rural hospitals have closed across 35 states, with a large concentration in southeastern states.1 Sadly, the rate of hospital closures is increasing: more rural hospitals closed in 2019 than in any year since 2005. And it isn't only hospitals that face closure. According to The Washington Post, over the last decade rural communities have lost 250 maternity wards, 3,500 primary care doctors, 2,000 medical specialists and hundreds of nursing homes.2
When a rural hospital closes, the entire community suffers. Hospitals often are the first- or second-largest employer in a small community, providing a vital economic boost to the local community. A hospital makes communities feel safer and provides much-needed community-based primary care, outpatient therapies and other health services. Local hospitals allow people to receive care closer to home, which is vitally important for seniors, people who do not have transportation, or people who cannot miss work for a doctor's visit. Additionally, larger employers who may want to invest in or relocate to a community may choose to go elsewhere if adequate health services are not available, thus perpetuating the cycle of economic decline for both the town and the hospital.
PUBLIC POLICY CHALLENGES AND OPPORTUNITIES
Perhaps the greatest burden faced by rural health care facilities is the regulatory burden placed on them by the Medicare Conditions of Payment and Conditions of Participation. For example, rural critical access hospitals must have a physician certify in advance that an admitted patient is expected to leave the hospital within 96 hours. Additionally, since a large percentage of new medical school graduates do not want to practice in rural areas, rural providers are disproportionately disadvantaged by the nationwide shortage of doctors, which exists largely because of the 1997-level limits on Medicare-funded residency slots that remain in place today. Further, rural providers are much more likely to face difficulty navigating the complex and disparate systems governing fraud and abuse rules, particularly as they relate to physician employment, patient transportation distance limits, and value-based bundled payment programs.
Many rural hospitals were built decades ago when the communities they served were larger, younger and healthier. Over time, rural hospitals have cobbled together new services to aid their aging patient base, closed floors or entire wings of their buildings, or made other changes to try to meet the needs of their patients. Unfortunately, however, there is no regulatory pathway for hospitals to downsize even further.
The two main types of rural facilities are small, rural hospitals and critical access hospitals. Both types have some special consideration given to them based on their status as pillar institutions within their rural communities. For example, small rural hospitals that have fewer than 100 beds may be classified as a "Medicare Dependent Hospital," based on their payer mix, or as a "Sole Community Hospital," based on the hospital's distance in relation to other hospitals. Both designations carry special Medicare reimbursement mechanisms. Critical access hospitals are unique in that they must have fewer than 25 beds, be located a specific distance from any other hospital, and operate under special Medicare reimbursement and Medicare conditions of participation. Critical access hospitals generally are paid at 101% of Medicare costs, minus the 2% withhold due to budget sequestration since 2013. For Medicare eligibility purposes, critical access hospitals must maintain an annual average length of stay of 96 hours or less for acute care patients. However, they are granted greater flexibility than traditional hospitals in their staffing requirements, such as the requirement that a physician must be available within 30 minutes in the case of an emergency.
Many small, rural hospitals would like to transition to critical access hospital status, but there is no easy path to do so under Medicare's guidelines. Critical access hospitals often were created through a governor's designation as a "necessary provider," but states have not been allowed to use that designation since 2008. Further, to transition to a critical access hospital, the hospital must be located in a state that has established a State Medicare Rural Hospital Flexibility Program, which a few states still have not done.
Additionally, some critical access hospitals would like to transition to become an even smaller facility, such as an emergency department with one or two inpatient beds, but, again, there is no mechanism to allow for this change without risking their current cost-based reimbursement. Instead, both types of rural hospitals are left operating in a manner appropriate to the situation they were built for decades ago rather than the situation they face today.
Rural hospitals need flexibility to meet the needs of their communities today, not the onerous requirements of Medicare or the needs of their communities in past decades. And we have opportunities! The Trump Administration has made regulatory relief a priority in its first three years, with calls for comments on antitrust rules, quality measurement requirements, nursing scope of practice and more. Engaging in public policy to help lift the regulatory burden could provide a way for rural hospitals to "right size" their facilities and services.
Many of the issues facing rural health care providers often tie back to one main problem: lack of available funding. The financial reality of critical access hospitals highlights the problem. American health financing is built largely on the idea that Medicare, Medicaid and other government payers will under-reimburse hospitals (and other providers) because the hospital can recoup these losses from the rates paid by private payers. But what if you do not have enough private payers?
For CommonSpirit Health, which was formed in February 2019 through the merger of Catholic Health Initiatives and Dignity Health, the Medicare population accounts for approximately 35% of acute care days in our hospitals, but the Medicare population accounts for an average of 60% of acute care days in our critical access hospitals. And while critical access hospitals are reimbursed differently by Medicare due to their special status, these hospitals do not get nearly enough reimbursement to cover the true cost of care. With significantly more than half of inpatient days paid through a system that under-reimburses providers, it is no surprise that the average critical access hospital in the U.S. operates with a total margin around 1.5%.
Public policy advocacy is the only way this dynamic will change. We can all use the resources of our system advocacy teams, national advocacy groups like the Catholic Health Association or American Hospital Association, and other membership organizations to ask our members of Congress to fully fund Medicare, to stop cutting reimbursement for providers and to support rural health care specifically. Additionally, we can ask for an end to budget sequestration cuts, which have reduced Medicare reimbursement by 2% for all hospitals, including rural facilities with cost-based reimbursement, since 2013.
Of course, under-reimbursement by Medicare is only part of the problem. Rural communities face higher rates of unemployment, and thus lower access to employer-based insurance, than their urban counterparts. In these areas, expanded access to government insurance is key. For example, in rural areas of states that have expanded Medicaid eligibility under the Affordable Care Act,3 the uninsured rate is 4 to 8 percentage points higher than the urban areas of the state; however, the uninsured rate in expansion states (both urban and rural areas) is significantly lower than that of non-expansion states. We know that people without insurance still get sick, of course, but they very often are unable to get preventive treatment because it is not available. By advocating for health care access and coverage for everyone, which is a key goal of Catholic health care, we can help make rural health providers more financially stable while also ensuring that those who are most vulnerable are able to access needed health services.
Payer mix and underfunding often lead to numerous other problems. For example, rural communities face serious workforce shortages due in part to financial woes and in part to regulatory restrictions. Rural hospitals are not as likely to attract new medical or nursing school graduates as urban areas. As a result, hospitals must entice clinicians to practice at their hospital, but are prevented from providing certain incentives by rules against overpayment and anti-kickback laws. The Centers for Medicare and Medicaid Services (CMS) recently proposed changes and asked for stakeholder input to improve some of these rules (known as the Stark Law and Anti-Kickback Statute). Individuals and organizations across the country were given the opportunity to provide feedback to the federal government on ways to improve the existing laws and, therefore, the overall health system. Regulatory comment opportunities like this are an excellent way to use public policy for the greater good.
Payment isn't the only barrier to a sufficient workforce, of course. Rural medical practices and hospitals need generalists in an era of medical specialty. They need greater leeway to use advanced practice providers, like physician assistants and nurse practitioners, for general medical services. Hospitals and clinics must have increased flexibility when hiring foreign medical graduates, both in terms of the number of visas allowed and the bureaucratic paperwork nightmare that comes when trying to hire these individuals. The federal government could utilize greater student loan paybacks to entice clinicians to rural areas. Loosening some of the regulatory burden around workforce would help reverse the trend of physicians opting for urban over rural practices.
This is where public policy continues to make a difference. Just last year, CMS finally ended rules that required a greater level of supervision for outpatient therapies than was required in the rural emergency room. This year, the federal government is seeking input on ways federal scope of practice laws prevent advanced practice providers from practicing at the top of their license and training. While these rules apply to far more than rural facilities, their positive impact on rural hospitals is disproportionately significant.
The challenges facing rural health care are discouraging, but as leaders in Catholic health care it is our privilege and responsibility to work toward a better health care system for everyone. By advocating with and for our rural brothers and sisters, we can use public policy to bring about positive change.
RACHEL C. TANNER is the system vice president of regulatory affairs and state relations for CommonSpirit Health. She is based in Denver.
NOTES
- Janie Boschma, "Record Number of Rural Hospitals Closed in 2019," Politico Pro Datapoint. See also Alya Ellison, "Rural Hospital Closures Hit Record High in 2019- Here's Why," Becker's Hospital CFO Report, Dec. 5, 2019.
- Eli Saslow, "Traveling the Loneliest Road," The Washington Post, Dec. 21, 2019, https://www.washingtonpost.com/national/traveling-the-loneliest-road/2019/12/21/f8ec26b2-21ca-11ea-bed5-880264cc91a9_story.html.
- "Health Insurance Coverage in Small Towns and Rural America – The Role of Medicaid Expansion," Rural Health Policy Project, https://ccf.georgetown.edu/wp-content/uploads/2018/09/FINALHealthInsuranceCoverage_Rural_2018.pdf.
QUESTIONS FOR DISCUSSIONRural communities are facing numerous threats to their survival, and the health care they need is at significant risk. More than 160 rural hospitals have closed since 2005; many more are in danger of closing because of financial instability. Rachel Tanner of CommonSpirit Health poses the question of what can and what should Catholic health care do to help the communities, patients and clinicians in such vulnerable situations. While the challenges seem overwhelming, Tanner thinks there are opportunities to update policy decisions, especially around the Medicare Conditions of Payment, to reflect the current realities of rural communities and their providers. - Rural communities may be served by either small, rural hospitals or critical access hospitals — both of which struggle with Medicare Conditions of payment. What can your system do to help rural facilities deal with the lack of funding they face? What kinds of community benefit support could help offset the inequitable Medicare conditions?
- Many recently licensed clinicians prefer to take positions in urban rather than rural settings. What educational support or residencies does your system offer to make rural placements more attractive? What ideas do you have in terms of tuition tradeoffs, paid internships, job security or other opportunities for new clinicians to help bring new talent to rural hospitals in your system?
- What do you think of Tanner's view of rural health care as an issue of justice at the ministry level (Catholic health care), the health care system level (your system and how it is advocating for its rural facilities) and the individual level (what you can bring to the table and how you can speak to your state senators and representatives)?
|