BY: MARK CRAWFORD
A key driver for improving patient satisfaction is "participatory medicine," in which highly engaged patients take an active role in their own health care management. It's also an inevitable and important step in the changing health care model and a critical aspect of patient-centered care.
"Most patients prefer to be more engaged," said physician Scott A. Wolf, DO, chief medical officer for Mercy Medical Center in Springfield, Mass. "Businesses also want their employees to be more engaged and proactive in understanding and managing their own health, because this ultimately leads to healthier and more productive employees, as well as decreases the cost of health care."
The terms "patient engagement" and "participatory medicine" are often used interchangeably in the medical community. However, participatory medicine takes engagement to a much higher level, one in which health care providers value patients as full partners.
Not all practitioners welcome the trend, however. Some resent it as a challenge to their education and experience; others view it as a time-consuming exercise in disabusing patients of notions they picked up on the Internet.
Nevertheless, asserted Ken Bertka, MD, vice president of physician clinical integration at Mercy Health Partners & Catholic Health Partners in Toledo, Ohio, patient engagement is vitally important as providers move toward patient-centered, value-based health care.
"In fact," he said, "the two most challenging aspects of health care reform will be payment reform and patient engagement."
A formal definition of participatory medicine by the Society of Participatory Medicine (www.participatorymedicine.org) describes it as a "cooperative model of health care that encourages and expects active involvement by all connected parties as integral to the full continuum of care."
"I would add that the entire multidisciplinary team should also be involved, across the entire continuum, including social workers, nurses, aides, volunteers, senior centers and family members, in addition to the patient," said Steve Moore, MD, senior vice president and chief medical officer of Catholic Health Initiatives in Englewood, Colo.
The foundation for participatory medicine is patients working closely with clinicians to become more knowledgeable about preventive care, as well as health maintenance and management of their own chronic conditions. They can then use this knowledge to make informed decisions in consultation with their physicians and other care providers. The process can also result in lower costs. This is, ideally, an ongoing relationship that depends on enhanced communication — often electronic — between patient and physician, "essential for reporting/discussing progress and/or problems with medications or other treatments," said Bertka. "It's also a good way to help patients realize that more medicine, more procedures and more expensive tests are not always the best solution."
GOOGLING FOR BETTER CARE
For Andrew Rose, MD, regional medical director for Bon Secours Medical Group in Richmond, Va., participatory medicine is both patient and provider working together as a team with the common goal of maintaining a long and healthy life. "This goal is best attained by utilizing all avenues available to the patient and the provider," Rose stated. "This includes research offline or online, in combination with the expertise of their medical provider and team."
Most providers have strong opinions about patients conducting their own medical research. Some physicians, especially those who like short meetings and want patients to simply accept what they say, regard self-educated patients as a threat to their authority; others worry about having to ward off dangerously misleading information. Everyone is acutely aware that detailed discussions during office visits about what a patient found on the Internet consumes ever-precious time.
"Some physicians may feel that patients will bog them down with questions or expect them to go over a stack of data from an Internet search," commented Janet Selway, DNSc, assistant professor and director of the adult nurse practitioner program at the Catholic University of America's School of Nursing in Washington, D.C. "Yet no single provider knows everything. We consult with each other as medical professionals; why shouldn't we consult with patients, especially if they find something that is helpful to their well-being?"
Zachary Meisel, MD, described just such a situation in his Jan. 19, 2011, article for Time entitled "Googling Symptoms Helps Patients and Doctors."1 Meisel wrote that he "saw a patient who came to the ER with a strange rash. She arrived with color printouts that correctly identified her condition. Not only was she correct in her self-diagnosis, but I am not sure I would have considered the right diagnosis so quickly if she hadn't brought in the pictures (it was a common condition with an atypical presentation). I know many health providers who have experienced similar circumstances."
Access to information — the key to engagement and participation — has never been easier. The Internet is a vast health care resource that can connect patients with others who have similar conditions and perhaps hold invaluable medical information regarding appropriate care. Engaged, motivated and well-informed patients often find information that providers don't have time (or reimbursement) to pursue.
On the other hand, one of the biggest issues that test the patient-physician dynamic is the terrible quality of some information patients often find on the Internet. Not only can it be dangerously wrong or have no basis in scientific evidence, it takes more time to discuss, especially if the physician is being challenged. Providers who are already stressed for time don't appreciate having their experience, training and expertise questioned by patients with no medical training, armed with printouts of misleading information, false claims and inappropriate or unproven treatments they found online.
"Physicians are indeed challenged at times by patients who have incomplete or inaccurate information, and think they can make as good or better decisions than the physician," said Bertka. "This is particularly true when the patient's knowledge is based upon the experience of a friend or family member, or inaccurate information from the Internet. The best thing to do is to keep communication lines open and be sure both the physician and patient understand what the other is saying."
Despite the concerns about dispelling misinformation patients bring in, or the extra time it takes, participatory medicine is a huge asset in the physician-patient relationship when done correctly.
AN EVOLVING PATIENT-PHYSICIAN DYNAMIC
"The days of the doctor telling a patient what to do and then moving on to the next one is becoming a practice of the past," said Rose. "I enjoy the fact that patients think for themselves; I want them to research and have as much knowledge as possible. Sometimes I learn something new. Patients who are inherently engaged usually have better outcomes to their care."
Those physicians and nurses working within the new model note that physicians can learn from patients as well as the other way around.
"I know first-hand, as a cancer survivor and from the many medical conferences I attend, that some doctors sneer or have the unscientific view that patients can't possibly know anything valid," stated David deBronkart, co-founder of the Society of Participatory Medicine, a public charity based in Minnesota. "I also know that an increasing number of docs — including mine — love it when their patients have a clue."
"Physicians must be prepared for a different kind of patient encounter," added Wolf. This includes being prepared to share/accept more information from well-informed patients, which adds a layer of complexity to the physician-patient relationship that requires patience, better communication skills and perhaps additional research.
Kathleen Sanford, RN, senior vice president and chief nursing officer at Catholic Health Initiatives, has seen an increased number of patients and family members with chronic conditions who bring a considerable amount of knowledge about their conditions to the office visit, which typically results in more detailed discussions with the medical team. "Patients may know more about their disease — especially if it is rare — than providers do," she said. "They certainly know more about themselves and how they react to various treatments. As a nurse, I've learned a great deal from patients about certain diseases, as well as what they need, as individuals, from us as providers."
FROM PASSENGER TO DRIVER
Empowerment can result in life or death — something deBronkart discovered after being diagnosed in January 2007 with late-stage kidney cancer. With a life expectancy of just six months, deBronkart rapidly learned to use every aspect of empowerment, technology and participatory medicine. Working closely with Daniel Z. Sands, MD, his primary care physician at Beth Israel Deaconess Medical Center in Boston and senior clinical informatics director for the Cisco Internet Business Solutions Group, they created an aggressive treatment plan that included surgery and High Dosage Interleukin-2 (HDIL-2). After months of grueling treatment, deBronkart beat the odds. Since September 2007, he has been cancer-free. This remarkable journey compelled Sands and deBronkart in 2009 to establish the Society for Participatory Medicine. Among its activities, the group publishes the peer-reviewed, open-access Journal of Participatory Medicine, www.jopm.org.
"Patients and families must be empowered and enabled to do more themselves," stressed deBronkart. "What we call the 'e-patient' movement — empowered, engaged, equipped, enabled — shifts networked patients from being mere passengers to responsible drivers of their own health, in which providers encourage and value them as full partners."
Empowerment/engagement begins with open, respectful and unrushed communication. Patients are encouraged to bring to their appointment a health history, a list of their medications and a list of questions and concerns. "Being open and honest with their physicians and clinical staff about what their main concerns and fears are, and what their personal goals are, is a key first step in establishing a participatory relationship," said Bertka. This honesty is especially important in order to delve into compliance and/or socioeconomic issues that may create barriers to optimal care.
Patients who are in a participatory relationship with their physicians and providers are encouraged to:
- Identify the information they'd like to have
- Learn how to find it
- Learn how to filter the "gold from the garbage" online
- Review what they find with their providers
- Connect with others who have their condition
- Keep track of important information about their conditions
- Maintain contact with key staff through electronic communications
FINDING GOLD, NOT GARBAGE
The Internet has given people the ability to find almost unlimited information about health, which can be a double-edged sword, warned Selway. "As health care providers we need to help filter information for people who may not know how to evaluate the quality of information they find or know the difference between strong evidence and weak evidence," she said. "People have a right to understand these concepts so that they can make informed decisions about their care."
According to the Pew Internet and American Life Project, 88 percent of U.S. adults with Internet access research health information and 60 percent of them have used this information to influence their health care decisions.
Their use of the Internet is also becoming more sophisticated. "In 2007, the most popular health-related website was WebMD," said Bertka. "Today, WebMD is second, having been surpassed by the National Institutes of Health's PubMed and MedLinePlus sites. Patients are starting to look for original research."
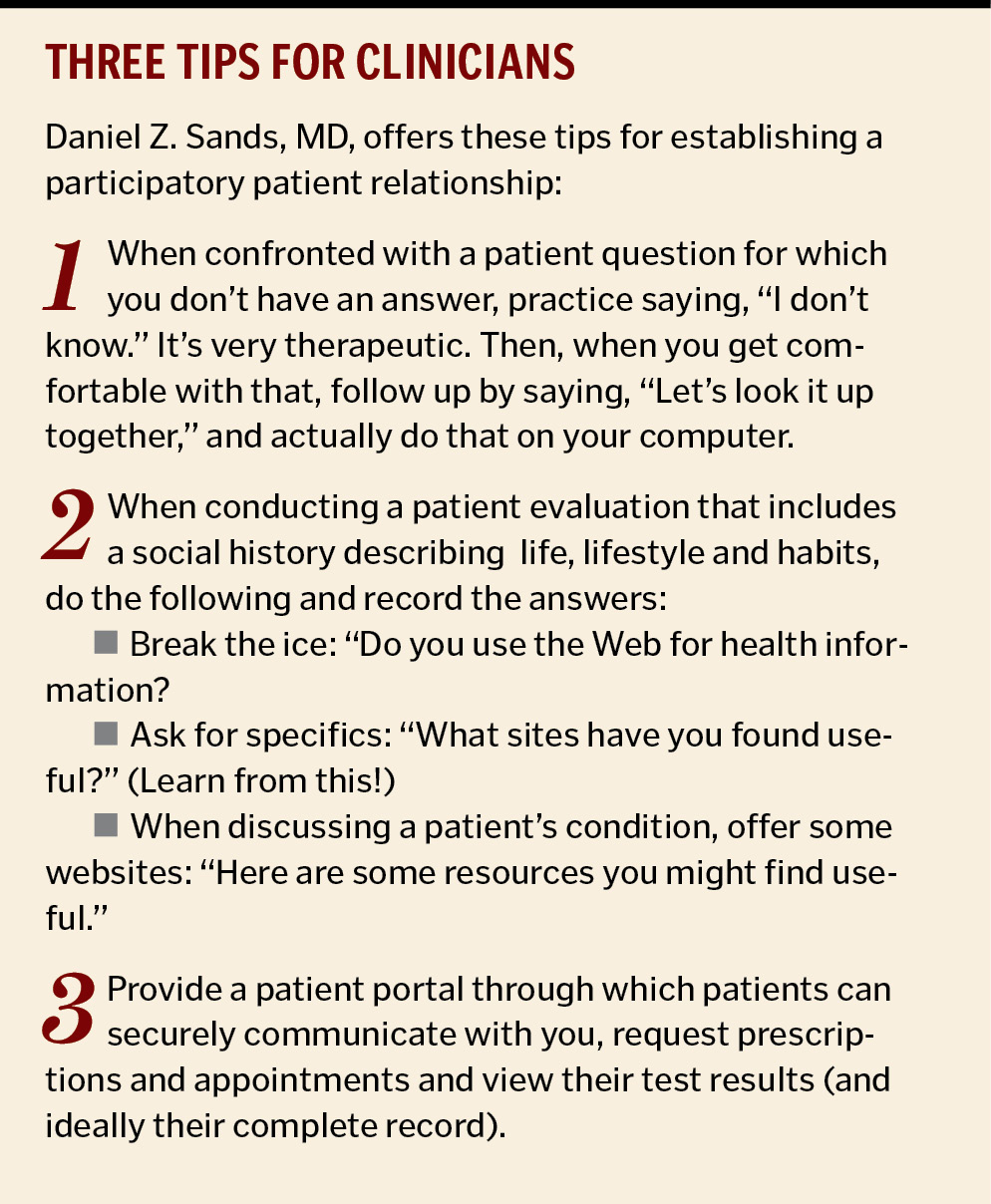
"Internet searching is not bad," Sands said, "but patients need to learn the attributes of good and bad websites." He pointed to the Medical Library Association (mlanet.org) as an example of a good source for educational information.
"I also encourage physicians to maintain a collection of generally useful websites for common conditions," he said. "This way they can always point patients to websites they trust to get them started on their searches. For many patients, that will be enough — for those who want more sophisticated information, we need to provide scientific papers and other material."
In addition to providing their own list of approved online sources, providers can "endorse and participate with companies that invest full time in creating resources for patient education, such as Emmi Solutions [a Chicago-based technology company], that enhance compliance and outcomes," Moore added.
GETTING WIN-WIN OUTCOMES
Participatory medicine is most effective when the appropriate IT assets are in place — this can be as simple as patient portals and email communication with patients. Sands co-authored the first guidelines/best practices for the use of email in patient care which provides guidance for addressing two interrelated aspects: effective interaction between clinician and patient and observance of medico-legal prudence.2
For participatory medicine to thrive, a robust electronic medical records system must be implemented that allows patients to communicate directly with providers and view their own charts. "We utilize a system called ConnectCare," said Rose. "Within this program is MYCHART. This function allows patients to have access to their charts. Utilizing these systems has allowed us to communicate more rapidly, accurately, directly and safely. Communication was a big gap in the past, but these technologies have allowed us to close the gap and improve patient outcomes."
The benefits of participatory medicine and working with engaged or activated patients are generally accepted throughout the health care industry, including:
- Improved preventive care, including cancer screenings and vaccinations
- Healthier lifestyles
- Reduced hospital readmissions
- Reduced medical errors
- Improved care coordination
- Decreased adverse outcomes from poor communication
- Improved adherence to treatment plans
- Improved smoking cessation
- Better chronic disease management
- Lower overall health care costs
"Better patient engagement is associated with better compliance, which leads to better outcomes," concluded Bertka. "Improved compliance with treatment early on and preventive care saves costs later. Additionally, if patients understand that more medicine and more tests are not necessarily better medicine, then unnecessary tests and treatments can be avoided, further reducing costs and complications of unnecessary treatments and procedures — a win/win for everyone involved."
MARK CRAWFORD is a freelance writer based in Madison, Wis.
NOTES
- Zachary Meisel, "Googling Symptoms Helps Patients and Doctors," Time (Jan. 19, 2011), www.time.com/time/health/article/0,8599,2043125,00.html.
- Beverley Kane and Daniel Z. Sands, "Guidelines for the Clinical Use of Electronic Mail with Patients," Journal of the American Medical Informatics Association 5, no.1 (Jan-Feb 1998): 104-111.
Copyright © 2012 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.