BY: WOODRUFF ENGLISH, MD, M.M.M., and TINA PICCHI, M.A., B.C.C.
The emerging role of spirituality within the discipline of palliative care re-energizes a commitment to more fully integrate spiritual care into mainstream medical care. As a result, Catholic health care is uniquely well-positioned to shape the transformation underway in the U.S. health care delivery system by preparing interdisciplinary palliative care teams to model whole person care for their professional colleagues.
Palliative care values and attends to the relational aspect of the whole person, the physical self, social self and spiritual self. It recognizes that each person has a spiritual center that suffers along with the diseased body. As a discipline, palliative care is committed to asking, "What do we need to know about you as a person to give you the best care possible?" and listening intently to patients' narratives to understand their worldview and what is most important to them.
Central to delivery of palliative care is an interdisciplinary team approach. The physician brings expertise in diagnosis and treatment of distressing physical symptoms and an understanding of prognosis. The nurse and social worker provide additional depth and support for the relationship stresses, grief and loss that come with serious illness. Chaplains assure a healing presence for the spiritual distress, fear and feelings of abandonment that often accompany unwelcome changes to the patient's functioning and life expectations.
Interdisciplinary palliative care teams spend a significant percent of their time engaging patients and families in goals-of-care conversations to ensure patients have a clear understanding of their disease process and treatment options. Often these conversations include decisions about preferred levels of medical treatment as their illness progresses. When palliative care practitioners are skilled communicators and spiritually grounded themselves, they are able to practice the art of presence and listen deeply to patients and families in a way that evokes trust among the care team, patient and family. This intentional commitment to discover, reverence and tend the spirit of another creates a numinous space where soul meets soul. This deepening of trust makes it possible for patients to give voice to their suffering, loneliness and fear as well as to their hope and aspirations for the present and future. It permits the care team to be honest and clear in their communications, helping the patient and family set realistic expectations for the time remaining. The goals-of-care conference itself can become a healing modality for the patient and a fortifying experience for palliative care professionals in overcoming burnout and compassion fatigue.
Chaplains, with their unique skills, have been underrepresented at these pivotal conversations with patients, families and other palliative care professionals and have not been used to full advantage as members of the interdisciplinary palliative care team. The power of their interventions has not been thoroughly recognized. The most recent data from the Center to Advance Palliative Care demonstrates that the median dedicated chaplain hours for hospital-based palliative care programs nationally is only 0.1 full-time equivalent, with a mean of 0.3 full-time equivalent.
PILOT PROJECT
The Supportive Care Coalition has committed itself to bringing a stronger presence of spiritual care into the practice of palliative care. We are sponsoring a nine-month pilot project to embed spiritual assessment and healing presence into the structure and design of the goals-of-care patient and family conversation. Five Supportive Care Coalition member sites are taking part (see sidebar), and each is required to have a palliative care chaplain participant in the project.
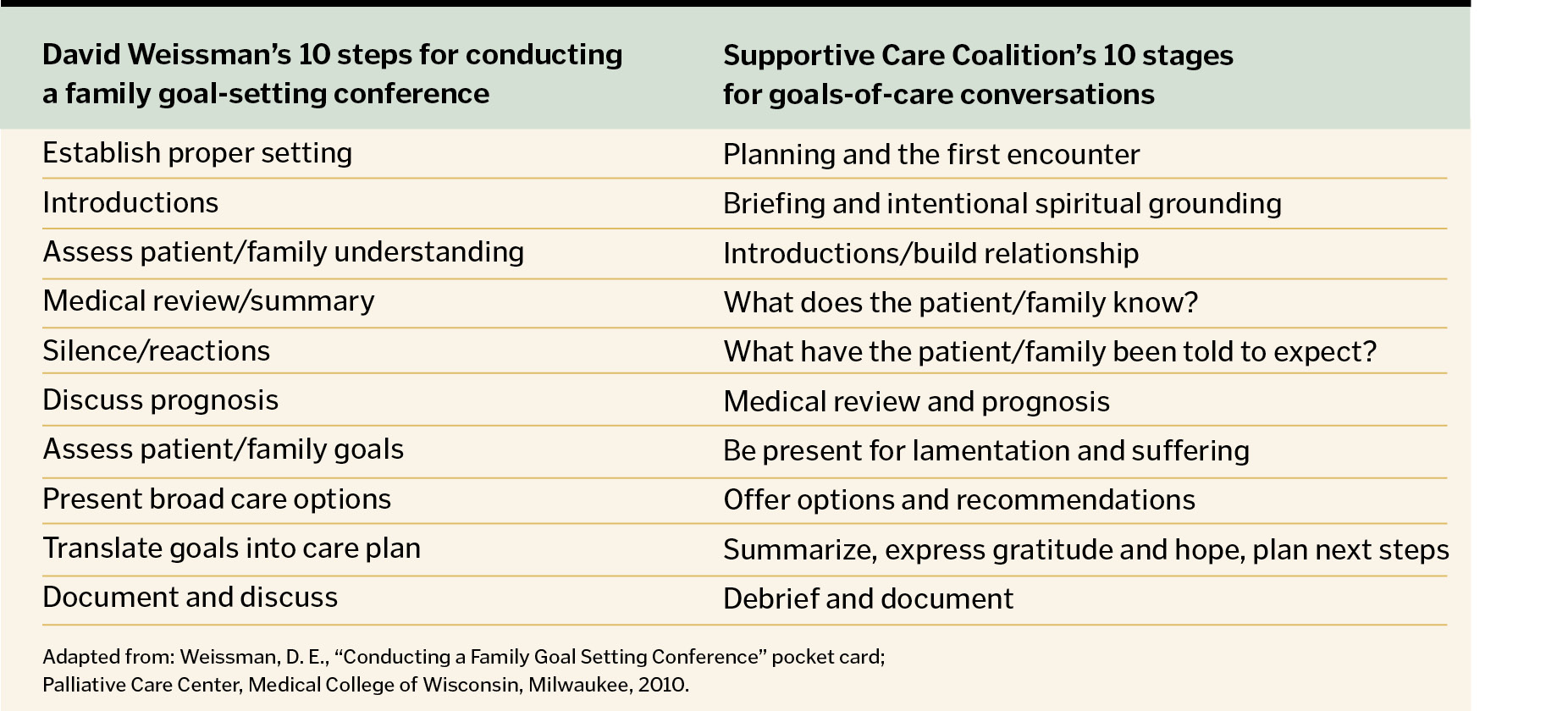
Our "Spirituality in Goals-of-Care Conversations" project's starting point is the 10-step guide for conducting goals-of-care conferences devised by David Weissman, MD.2 (See sidebar). With his permission, we have modified his methodology to place greater emphasis on preparing both the care team and the patient and family for this conversation, identifying sources of hope and spiritual strength, as well as attending to spiritual suffering, loneliness and fear.
In November 2013, the pilot project teams gathered in Portland, Ore., for a training program that focused on listening intently for the voice of the soul in conversations with seriously ill patients and their loved ones. Physicians, advanced nurse practitioners, RNs, social workers and chaplains explored spiritual practices that could inform and strengthen their capacity to build trust and deepen relationships not only with patients and families, but within the care team itself.
Using a quality improvement model, the pilot project aims to increase interdisciplinary palliative care teams' competence in recognizing and addressing spiritual suffering and integrating the patient's beliefs and values into advance health care planning. Baseline data revealed that our project teams were satisfied that goals-of-care conferences integrated the patient and family's spiritual concerns, beliefs and values into their treatment discussions 37 percent of the time. We expect this will increase significantly as these teams implement the project tools and resources, including team preparation and spiritual grounding and debriefing practices, as well as suggested scripting. Over the course of the project, we will make refinements and replicate a successful training experience that can be shared with other Supportive Care Coalition member organizations and disseminated to the broader palliative care community. We will present an evaluation of the project at our board of directors' strategic planning retreat in fall 2014.
This project is the result of two strategic initiatives endorsed by the Supportive Care Coalition's board of directors. The first is to bring spiritual wisdom to the care of the seriously ill, with an interdisciplinary team approach to meeting spiritual needs and relieving spiritual suffering. The second is to help palliative care teams cultivate an appreciation of their vocational call to service and to foster personal and professional commitment to spiritually grounded values that will sustain them in their care of persons who are suffering.
To oversee the implementation of these initiatives, our board of directors appointed a spirituality steering committee devoted to helping our palliative care colleagues be present to the suffering and lament of those who struggle with religious, spiritual and existential pain.
Committee members worked together for more than 18 months, discerning how to integrate spiritual practice into the core work of interdisciplinary palliative care teams. Several elements surfaced in the committee's discernment:
- How does a palliative care clinician learn to listen deeply for the voice of the soul?
- How do we approach serious illness in the context of modern-day cultural values?
- What can we learn from the wisdom of our elders and ancestors in the way they understood and treated serious illness?
A seminal article in the New England Journal of Medicine by Eric Cassell, MD, emeritus professor of public health, Weill Medical College of Cornell University in New York City, has informed our work. Cassell examined the nature of suffering and its relationship to disease, noting that failure to understand it can result in medical intervention that not only fails to relieve suffering but becomes a source of suffering itself. He described the many aspects of personhood that are susceptible to damage and loss in the experience of profound illness.
Published in 1982, Cassell's article was transformational in that it brought the bio/psycho/social/spiritual model of care to scientifically oriented readers through its wide dissemination.3
Ira Byock, MD, author of The Best Care Possible: A Physician's Quest to Transform Care Through the End of Life and a keynote presenter at the 2013 Supportive Care Coalition Congress and Catholic Health Assembly, speaks passionately about transforming care through the end of life and the intrinsically spiritual nature of caring for the seriously ill.
"The confrontation with death lays bare the spiritual core of the human condition," he says. "The force of impending death acts like a hot wind to strip away all pretenses and expose each person's elemental essence. What we call spiritual is our innate response to the awe-inspiring and terrifying mystery of human life and the universe. ...Confronted with the mystery of life and death, we reflexively try to make some meaning of our experience in the world, strengthen our relationships with others, and feel part of something larger and more enduring than ourselves."
Byock expresses a truth that resonates with many palliative care professionals as they contemplate their work with the dying and their loved ones: "For all the suffering that surrounds dying and death, many people experience such times as sacred."4
SPIRITUALITY
At the 2009 Consensus Conference, "Improving the Quality of Spiritual Care as a Dimension of Palliative Care" in Pasadena, Calif., 40 national leaders including physicians, nurses, psychologists, social workers, chaplains and clergy, other spiritual care providers and health administrators, made recommendations to advance the delivery of quality spiritual care in palliative care. They produced a definition of spirituality based on considerable research and expert opinion. It states: "Spirituality is the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred."5 Recognizing the strengths and limitations of this consensus definition, our board of directors accepted this definition of spirituality, viewing it from a Catholic theological perspective.
This definition was included in the 2013 National Consensus Project's 3rd Edition of the Clinical Practice Guidelines for Quality Palliative Care.6 The NCP guidelines are endorsed by numerous national health care organizations. They describe the core precepts and structures of clinical palliative care programs, promote consistent and high quality care and reflect the growing practice and evidence of palliative care as it continues to move into mainstream health care.
The guidelines recognize spirituality as a fundamental aspect of compassionate, patient- and family-centered care that honors the dignity of all persons.
The guidelines place an emphasis on the responsibility of the interdisciplinary team, inclusive of an appropriately trained, preferably board-certified chaplain, to explore, assess and attend to the spiritual issues of the patient and family. They highlight education and training necessary to address spiritual suffering and promote spiritual and religious rituals and practices that are sensitive to cultural and religious diversity.
Parker Palmer, in his 2004 book, A Hidden Wholeness: The Journey toward an Undivided Life, offers palliative care a way to elicit the patient's narrative from a deep place using a traditional method for being present and listening intently for the voice of the soul (or the inner teacher) to speak.
Coming from the Quaker tradition, Palmer reflects upon how circles of trust create a safe and contained place in community for individuals to get in touch with their "inner teacher." If the inner teacher can speak to a person, the individual can become grounded in who he or she is and, in a very deep way, become more intentional about how they make decisions for their life. This presupposes that members of the community who form the circle of trust are also in touch with their own inner teacher or soul and speak genuinely from within in their conversations with this individual.
"When the space between us is made safe for the soul by truthful speaking and receptive listening, we are able to speak truth in a particularly powerful form … as we tell the stories of our lives …passing along our traditions, confessing failings, healing wounds, engendering hope, strengthening our sense of community … In our culture of invasion and evasion, this time-honored practice cannot be taken for granted. It must be supported in special settings and protected with strong ground rules."7
Palliative care is a time-honored practice and seeks to provide the special and protected setting that Palmer refers to when he speaks of circles of trust. In recent years, palliative care professionals at Providence Health & Services in Portland, Ore., have adapted these circles of trust in their approach to goals-of-care conversations. As a result, they have become more spiritually grounded, receptive and present to patients, and their conversation often moves to a profound level.
These palliative care physicians and their interdisciplinary colleagues pay more attention to the patient's narrative, inquiring how illness has changed or disrupted his or her life and relationships and how this experience has impacted their values, sense of meaning and purpose, justice and fairness and the role that death and transcendence plays in their belief system. This allows the palliative care team to discover what the person truly values, drawing upon the patient's "inner teacher" as a guide to construct a medical care plan that meets the person's needs in a deep and intimate manner.
Spiritual wisdom is very broad, with many spiritual traditions that provide important knowledge, interconnection and pathways to explore. Each holds a fundamental belief that there are things beyond our comprehension that pertain to the realm of mystery. We draw upon essential common principles and universal threads of experience, woven in a rich tapestry of cultural diversity and ancient truths. In the context of palliative care, we recognize that our interactions with patients and families are sacred encounters and, as such, must be treated with respect and approached with humility.
WOODRUFF ENGLISH, MD, is the clinical project leader for the Spirituality in Goals-of-Care Conversations Project. Recently retired, he was the palliative care medical director for Providence Health & Services, Oregon Region, and a member of the Supportive Care Coalition board of directors.
TINA PICCHI is executive director, Supportive Care Coalition, Hillsboro, Ore.
NOTES
- Center to Advance Palliative Care, "The New National Palliative Care Registry: Making the Data Work for You," webinar presentation, Dec. 5, 2013.
- David E. Weissman, "Conducting a Family Goal Setting Conference," laminated pocket card, Palliative Care Center, Medical College of Wisconsin, Milwaukee.
- Eric J. Cassell, "The Nature of Suffering and the Goals of Medicine," New England Journal of Medicine, 306, (March 18, 1982): 639-45.
- Ira Byock, The Best Care Possible: A Physician's Quest to Transform Care Through the End of Life (New York: Avery, 2012), 291.
- Christina Puchalski et al., "Improving the Quality of Spiritual Care as a Dimension of Palliative Care: The Report of the Consensus Conference," Journal of Palliative Medicine 12, no. 10 (2009): 885-904.
- National Consensus Project for Quality Palliative Care, Clinical Practice Guidelines for Quality Palliative Care, 3rd edition (Pittsburgh: HPNA, 2013).
- Parker J. Palmer, A Hidden Wholeness: The Journey toward an Undivided Life (San Francisco: Jossey-Bass, 2004), 122-23.
PILOT PROJECT PARTICIPANTS
The following Supportive Care Coalition member organizations participated in the palliative care pilot project:
Borgess Medical Center, Kalamazoo, Mich. (Ascension Health)
Providence Little Company of Mary Medical Center, Torrance, Calif.
Providence Sacred Heart Medical Center, Spokane, Wash.
St. Mary's Hospital, Richmond, Va. (Bon Secours Health System)
St. Thomas West Hospital, Nashville, Tenn. (Ascension Health)
THE SUPPORTIVE CARE COALITION
The Supportive Care Coalition, composed of 22 Catholic health care organizations, is dedicated to advancing excellence in palliative care. Founded in 1994, the group shares a common vision and belief that palliative care is a hallmark of Catholic health care, and it partners with other national organizations committed to improving the quality of life for persons living with serious illness.
As a faith-based organization, the coalition aspires to make a significant contribution to the field of palliative care by identifying and promoting leading practices that bring spiritual wisdom to the care of the seriously ill and spiritual care resources to palliative care professionals. The goal is to honor the unique spirituality of each patient and family, identify and attend to spiritual suffering and help each individual draw upon his or her own spiritual strengths and resources for healing and wholeness.
Members of the coalition are equally committed to the spiritual health and well-being of palliative care staff and to their spiritual growth and formation.