BY: JANE DURNEY CROWLEY, M.H.A.
Every five years, Catholic Healthcare Partners (CHP) brings together a multi-disciplinary team of leaders, representing all nine of our regional health systems, to engage in facilitated strategy sessions to help set the system's strategic direction for the coming fiveyears. The results are presented to the CHP Board of Trustees in draft form, and after reviewing, editing and sometimes re-focusing, the board votes to accept the strategic direction and our executive management team is then responsible for seeing it through successfully.
Always grounded in our mission, CHP's strategic direction is designed to help our system, as President and CEO Michael D. Connelly puts it, "meet infinite needs, with limited resources and diverse points of view."
And given that the majority of our regional health systems are in historically economically depressed geographic areas, we believe that we've gotten very good at delivering high quality care while providing great value. But last year, we were challenged in a way that we've never been challenged before.
CHP's Strategic Direction 2009-2013 was in the final edit in the fall of 2008 when the international financial meltdown began in earnest. We were also finalizing the annual plan for 2009, including the system and regional health system objectives, operating budgets and capital budgets. Having a stable infrastructure in place, our Lead the Ministry Team — a team of system-level executives — was able to move quickly to evaluate our annual and strategic (long-range) plans against the hard realities of investment losses, credit tightening and the impending recession.
In this article I will reflect on the impact of the financial market dislocation in 2008 and the recession of 2008-2009 on CHP's planning processes; the choices we made; and the implications for the ministry as we head into a period of rapid transformation.
TACTICAL DECISIONS FOR 2009
As many have observed, this recession was clearly deeper than others we have recently experienced. Sizeable investment portfolio losses in the fourth quarter of 2008 all but confirmed that the country was in what would turn out to be a serious recession with crushing job losses. To weather the storm and ensure that we can continue to successfully carry out our mission, the Lead the Ministry Team adopted twin adaptive strategies: preserve cash and reduce operating expenses.
The team reduced the capital budgets for 2009 and 2010 by $170 million or 23 percent over the two years. To accomplish this, some large projects such as a replacement facility for a rural hospital were "bumped" out a year; other projects such as the construction of a new hospital were trimmed; but replacement capital was maintained at a minimum base level for each regional health system. The team established a contingency to provide for unexpected needs. Other cash preservation tactics included deferring pension funding and optimizing the timing of accounts payable. In total, these moves allowed CHP to add back 27 days to Days Cash On Hand.
Tight integration of strategic and financial planning teams and tools made it possible to make these changes so late in the annual planning process. Our capital planning cleanly segregates replacement capital from strategic initiatives, allowing us to delete, change, or add strategies and easily calculate the impact on the annual plan and five-year strategic direction.
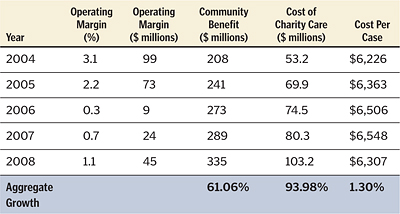
Our multi-pronged approach to reducing operating expenses included regional health system cost control, eliminating or reducing incentive compensation despite strong operating results and reducing system educational events and home office expenses. The result of these changes, on top of robust cost management systems already in place, has allowed CHP to reduce its cost per unit of service by 3.8 percent in 2008 compared to 2007, and we're expecting no increase in cost per unit in 2009. Cost control has been the lifeblood enabling us to continue to serve all in need as the cost of charity care in our facilities rose 29.2 percent in 2008 alone, continuing a multi-year journey as well.
CONFIRMING AND ACCELERATING TRANSFORMATIONAL STRATEGIES
CHP believes strongly that a period of rapid and radical transformation of health care delivery already has begun. As we pursued an immediate and aggressive tactical response to the economic crisis, CHP also reevaluated, reaffirmed and accelerated investment in transformational strategies. These include: partnering with our physicians to produce higher quality, better coordinated, more efficient care; rapid deployment of health information technology within our delivery system and the broader community; and large-scale reductions in variation in quality care delivery and in harm and waste associated with inpatient care. These strategies were already contained within the CHP Strategic Direction, but during the many serious and challenging days of the fourth quarter of 2008 and the first half of 2009, we found ways to redouble our efforts.
STRENGTHENING ALIGNMENT AND ACCOUNTABILITY AT THE BASE OF THE HEALTH SYSTEM
The predominant model of physician practice in CHP communities remains small, single specialty, private practice. CHP facilities have enjoyed a long and productive relationship with our affiliated physicians, yet the constraints of this model are increasingly evident to both hospitals and physicians. Hospitals seek means to align physicians with the quality and efficiency outcomes for which we are responsible (evidence-based medicine compliance; avoidance of harm; cost control) and to prepare for new responsibilities — care coordination for chronically ill and care of populations. Physicians seek lifestyle balance, financial security and the capital necessary to upgrade office practice technology. CHP's strategic plan calls out three physician engagement strategies: improving the supply of primary care physicians in our communities; bolstering the practice infrastructure for our employed physician practices; and restructuring and supporting the core set of physician relationships — community-based primary care physicians, emergency department physicians, and hospitalists. This last strategy is transformational.
CHP used the talents of our systemwide Leadership Academy class to develop a template of best practices for emergency department and hospitalist physician performance-based contracts. Many hospitals continued or initiated their development of formal hospitalist programs. And teams are researching the existing and desired means of communications among the members.
In 2010, we expect to renegotiate contracts to include performance expectations as well as pilot structures for supporting the team of physicians at the base of most hospital admissions. With the advent of hospitalist medicine as a subspecialty, the roles and communications of the three groups of physicians have been altered. We hope to create a forum for role clarification, issues resolution and care coordination for the three groups, recognizing that these three groups are responsible for the majority of care for most hospital patients. We expect the outcome of this work to be multi-faceted: improved physician satisfaction, better care coordination, and reduced harm (errors and readmissions).
STANDARDIZING HEALTH INFORMATION TECHNOLOGY
The strategic direction commits CHP to adopt a standard clinical information system for inpatient and ambulatory settings within five years, investing $250 million over that period. For our strategy, called CarePATH (PATH stands for Patient-centered Access to Team-based Healthcare), CHP has partnered with Epic Systems for advanced clinical information technology in both inpatient and ambulatory settings (emergency department and physician practices) throughout our system. The stimulus bill passed in February 2009 caused us to adjust our timing and re-sequence certain installations to maximize the achievement of "meaningful use" and the eligibility for additional reimbursement. The first physician practices, Mercy Medical Associates (Cincinnati) went live on CarePATH in November 2009, and in February 2010, Mercy Hospital Fairfield, Ohio, will be our first hospital to go live.
Further, Cincinnati is blessed with a nationally recognized Health Information Exchange called HealthBridge, franchised to Springfield, Ohio, in 2008 with CHP's help. CHP has made a commitment of $250,000 in each of the communities we serve to assist with the start-up of such health information exchanges where one currently does not exist.
While the stimulus money will help CHP fund and accelerate our health information technology strategy, we were already committed to full deployment of advanced clinical informatics to support our drive to transform our health care system to one of seamless, team-based care to meet the needs of those we serve.
RADICALLY REDESIGNING INPATIENT CARE
CHP's metrics in quality and efficiency are trending very positively. In fact, CHP was recognized as fifth in the nation when it comes to high quality health care in a report published in the June 2008 issue of the Joint Commission Journal on Quality and Patient Safety. The study compared 73 hospital systems using data publicly reported by the Centers for Medicare and Medicaid Services. Additionally, in 2009, CHP was honored as a Top 10 health system for quality in efficiency in a Thomson Reuters study of 252 health systems across the country.
But until no harm occurs in any of our hospitals, and all patients receive the highest quality of care at all times, CHP knows that we cannot rest. Planning for the next five years during this very difficult time presented the perfect opportunity to recommit to and focus on continued improvements in quality and safety processes.
CHP's efforts to eliminate harm in its hospitals have been multi-faceted and continuous since at least 2005. Major areas of focus for improvement include:
- A focus on the Institute for Healthcare Improvement's 5 Million Lives campaign targets, including adverse drug events, surgical complications, reducing pressure ulcers, reducing infections and delivering evidence based care for heart failure
- Early sepsis recognition and treatment to prevent mortality
- Falls with trauma through nursing innovations
- Obstetrical care by implementing five evidence-based practices
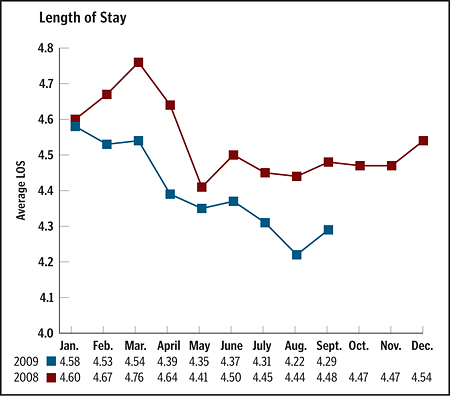
Organizational strategies have included Lean Six Sigma training and tools, learning collaboratives, evidence-based medicine and nursing order sets, rapid response teams, formal WalkRoundsTM, TeamSTEPPSTM, and Patient Safety Academies. More recently, the redesign work has focused intently on patient flow and care coordination. Visual control systems have been installed in five hospitals, and the case management departments have been redesigned in seven facilities at present. The clinical results have been significant, and the cost of care has been reduced dramatically — and risk-adjusted length of stay has been reduced by 5 percent since 2007.
Thanks to sometimes tough long-term and short-term strategic and tactical decisions, CHP was able to support a strategy to redesign care to prevent harm and reduce waste despite an unplanned hit to our investment portfolio, ever-increasing demand for uncompensated care, and the certainty of impending cuts to public funding (Medicare, Medicaid). As our journey continues, we will do all we can to be faithful stewards of our limited resources, so that we can continue fulfilling our mission and improving the health of the communities we serve.
JANE DURNEY CROWLEY is executive vice president and chief administrative officer, Catholic Healthcare Partners, Cincinnati.
ABOUT CATHOLIC HEALTHCARE PARTNERS
Catholic Healthcare Partners is the largest health system in Ohio and one of the largest not-for-profit health systems in the U.S. With $4.76 billion in assets, CHP employs 36,500 associates in more than 100 organizations, including 32 hospitals which serve people in Ohio, Tennessee, Kentucky, Pennsylvania and contiguous states. In 2008, CHP provided more than $335 million, or 8.2 percent of total expenses, in targeted community benefit. In 2009 CHP was honored as a Top 10 health system for quality in efficiency in a Thomson Reuters study of 252 health systems across the country.
Copyright © 2010 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.