Mark Repenshek, PhD
Healthcare Ethicist
Columbia St. Mary's
Milwaukee, WI
[email protected]
In October of 2010, the American Association for Bioethics and the Humanities (ASBH) released for publication Core Competencies for Health Care Ethics Consultation.1 The document is a follow up to the 1998 report. This seminal work identifies the core competencies essential for doing quality health care ethics consultation and education. This most recent edition solicited commentary from the field prior to its final release. These efforts have produced a document that addresses a number of important issues in the field, for example: eliminating unhelpful distinctions on the types of work done in ethics and moving to a more seamless transition from clinical ethics to organizational ethics; broadening the document beyond a sole focus on clinical consultation toward better examining the scope of health care ethics; and examining quite closely the issue of emerging standards in the field along with continuous quality improvement.
It is this last area that I wish to address and, in doing so, provide a tool that will allow Ethics Committees to communicate effectively in the quality arena through the use of a "Dashboard (See addendum)."
Since 2003, Columbia St. Mary's has utilized a method of tracking ethics consultation that continues to evolve. The Microsoft Access database Ethics Tracker, created by Harmony Technologies, LLC, provides us with the capability to examine the questions related to continuous quality improvement of our ethics consultation service. I have published on the capabilities of Ethics Tracker in the past.2 This article will focus on the creation of a "Dashboard" template within Ethics Tracker to crosswalk quality improvement initiatives in ethics with the ASBH 2010 Core Competencies for Health Care Ethics Consultation.
In Aulisio and colleagues' 2003 edited work, Ethics Consultation: From Theory to Practice, Jacqueline Glover and William Nelson provide a compelling chapter on innovative educational programs in ethics. They argue that such programs are a necessary first step toward improving quality in ethics consultation.3 Given the variance in what one means by ethics consultation, Glover and Nelson remind us that we need to start with a baseline set of competencies with regard to which committee members can demonstrate proficiency in order to begin to talk about quality improvement. Or, in their words, "What specific training should these individuals [who do ethics consultation] possess to function effectively as an ethics consultant?"4 Yet, despite this call, use of the ASBH Core Competencies as a way to establish that baseline seems to still remain only a plea. Colleagues at the Veterans Health Administration continue to offer substantive work in this area and thus are featured prominently in the 2010 ASBH document. That said, even an opening letter from the Chairperson of the Core Competencies Update Task Force acknowledges, "in many instances, no other published resources were located that were as comprehensive as the VA's."5 This in no way intends to diminish the work; rather it is a "call to action" of sorts on the part of the field to remain in dialogue in order to contribute to a conversation on continuous quality improvement.6 In Catholic health care, this call is just beginning to be heard.
The collaborative effort between the Catholic Health Association and Ascension Health on the document Striving for Excellence in Ethics is an attempt to stretch the resources provided by ASBH and the VA's National Center for Ethics in Health Care. The resource is intended to "identify core components of a robust ethics services, and for each component, suggest "standards" that, if implemented, would enhance that particular component."7 Still, the tool is an assessment and is therefore limited. It is designed to evaluate where a program is at, but offers little direction in terms of what steps a program should take when concerned with quality improvement. But, returning to Glover and Nelson's critically important point, evaluation is an absolute necessity for continuous quality improvement. I offer the following metrics as important starting points for continuous quality improvement initiatives in ethics, utilizing a "Dashboard" template for efficient communication throughout an organization. I will also use categories drawing from the ASBH Core Competencies document for structuring an Ethics Dashboard. Finally, in each category a particular criterion is highlighted in yellow. These criteria have been chosen by our ethics committees as "critical measures of success" within the broader categories.
Ethics Committee Structure and Function
There is a wealth of literature that has surveyed ethics committees for over ten years. Data from these surveys suggest that ethics committee structure and function is highly variable.8 To illustrate this point, although it is generally agreed upon that an ethics committee should be interdisciplinary in nature,9 the ASBH Core Competencies document recognizes that "ideally, there would be research linking specific structural standards with the achievement of desire goals or outcomes. Unfortunately, such data are almost entirely lacking."10 Here, again, Glover and Nelson's work is incredibly important. To restate their claim more succinctly, we need to start measuring something before we can ever begin to discuss improvement. If being interdisciplinary is a recommendation of the Core Competencies, the field should begin to define the optimal number of disciplines that constitutes interdisciplinary. Once defined, we can then begin to link goals with structure.
Table 1
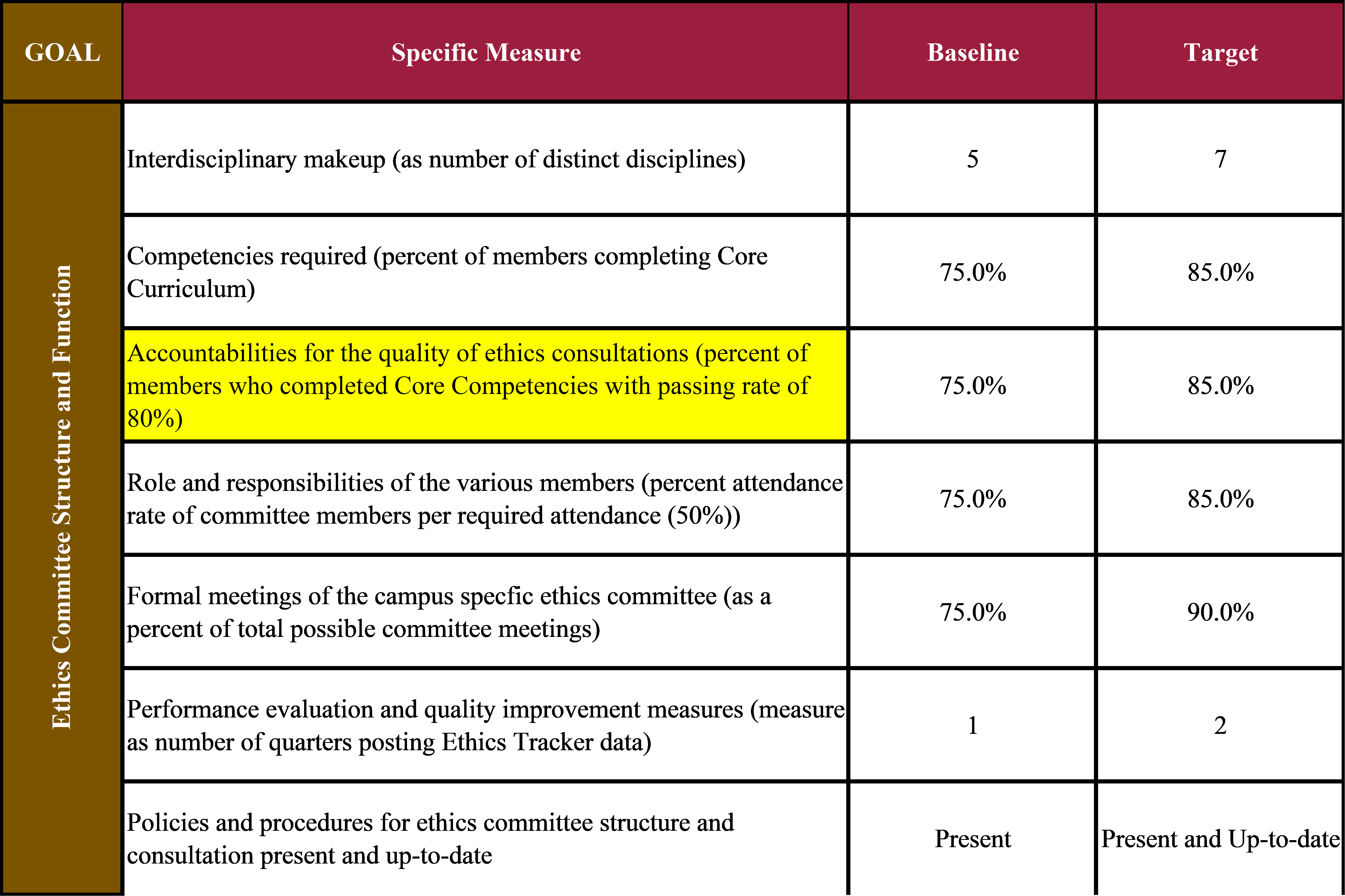
Using the idea of baseline and target to establish where we need to be and where we want to be, respectively, Columbia St. Mary's Ethics Committees have made the claim that to be truly interdisciplinary at least five distinct disciplines are required when considering ethics committee membership (Table 1). By distinct disciplines our committee policy does not allow for a physician member who is a nephrologist and a physician member who is a pulmonologist to be considered "distinct." Rather both would be considered a physician member.
Glover and Nelson feature a number of innovative educational programs designed to educate ethics committee members on a set of core skills and knowledge sets necessary for ethics committee membership.11 As a ministry of Ascension Health, Columbia St. Mary's ethics committees have the benefit of access to Ascension Health University. Within this web-based resource, we are able to access eight ethics modules with pre- and post-tests to demonstrate learning. As part of the university, transcripts are able to be produced and linked with Continuing Medical Education (CME) adding an additional incentive. Most importantly, in terms of continuous quality improvement, the ethics committee can determine for its membership the level and standard by which their competency will be assessed. Our ethics committees chose a passing rate of 80% as a threshold requirement for anyone wishing to be part of the ethics consultation teams. From this starting point, the ethics committees at Columbia St. Mary's then set standards for the level of competency across the entire committee (in our case 85% of total committee membership as our target rate). Additional items related to structure and function comprise attendance, number of formal meetings of the ethics committee per year (necessary forums for continuous self-improvement), posting of ethics committee quality data as a matter of transparency, and policy updates.
Ethics Consultation Service
A major component of the ethics consultation service is the ethics consultation provided to patients, families, physicians, nursing, and any direct care provider of the patient. The ASBH Core Competencies defines the consultation service as, "a set of services provided by an individual or a group to help ... address uncertainty or conflict regarding value-laden concerns that emerge in health care."12 Given the integral nature of ethics consultation to the work of an ethics committee, it would seem there is great opportunity for a link between specific standards and the achievement of a desired goal or outcome as called for in the Core Competencies. Relying heavily on work done by Douglas Opel at the Treuman Katz Center for Pediatric Bioethics, our ethics committees track ten areas for documentation of ethics consultation.13 Quality ethics documentation within the EHR is essential for communication of ethics consultation and the associated recommendations from clinician to clinician, shift-to-shift.14 Finally, upon completion of data entered into Ethics Tracker, an email is automatically generated to the individual who requested ethics consultation in order to obtain feedback on the timeliness and overall benefit of the service (Table 2).
Table 2
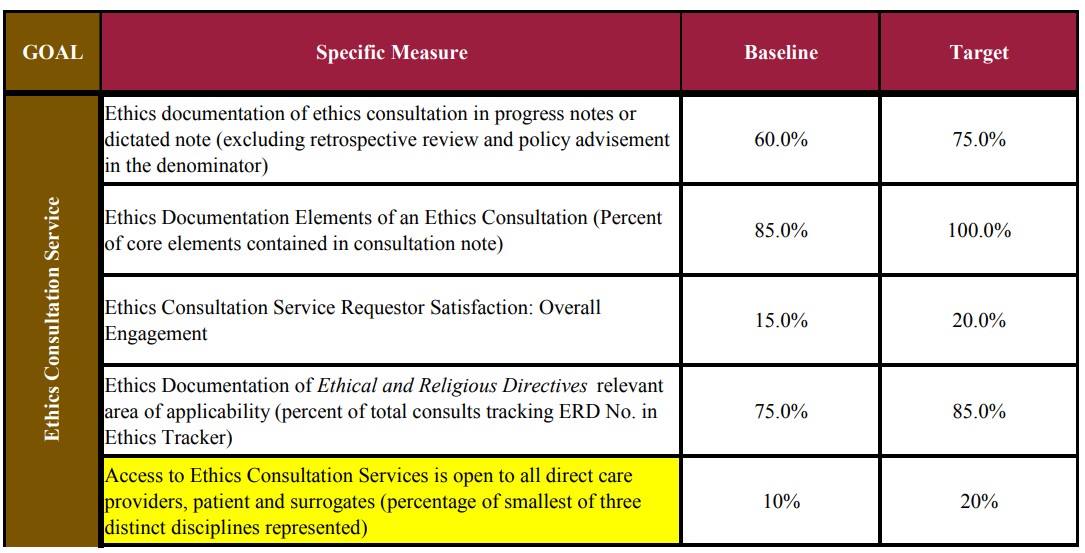
As a Catholic health system, it is also critical that we continue to make an explicit link between the ethics consultation service and use of the Ethical and Religious Directives for Catholic Health Care Services (ERDs) as a foundational tool for insight and education. In order to develop this link, a crosswalk was created between the "Reason(s) for Consultation" standard to our database and a set of corresponding Directives. Tracking the relevant Directives to the case allows for greater familiarity with the Catholic tradition in health care ethics for all parties involved: consultant, committee and health care team.
Finally, recognizing that accessibility is a key determinant for any quality ethics consultation service, our ethics committees desired a measure that would reflect multidisciplinary request.15 The committees chose to use the percentage of the smallest of the top three distinct disciplines of requestor in Ethics Tracker to measure organizational access. That is, 10-20% of ethics consultations (baseline and target, respectively) should be represented in the third highest discipline of request whether that is nursing, case management, physician or some other direct care provider discipline. Tracking this measure allows us to quantify the extent to which multiple direct care providers feel comfortable utilizing the ethics services or to what extent ethics services may be stifled on a particular unit. Clearly there is significant room for debate on this measure, but again, to Glover and Nelson's earlier point, when we begin to measure the degree of organizational spread for our services then, and only then, can we begin quality improvement related to access.
Ethics Consultation Service Effectiveness
This section presents perhaps the most significant contribution to the dialogue concerning quantifiable measures for ethics consultation service effectiveness. The ASBH Core Competencies make six recommendations in this area none of which suggest actual measures. To be clear, the recommendations are critically important, but the lack of both practical suggestions and limited reference to the literature demonstrates the difficulty with establishing what constitutes "service effectiveness" in ethics consultation. Our proposed criteria move away from the ASBH Core Competencies a bit in that these measures are less about outcomes based on "conflict resolution"16 or "satisfaction"17 and more about measuring the outcomes based on set claims of what constitutes a quality ethics consultation.
Our first criterion is an example of our desire to move away from satisfaction as it may or may not be perceived by the parties involved with ethics consultation and is rather about moving consultation earlier into the patient stay (Table 3). A couple of assumptions should be acknowledged here. The earlier ethics is involved in the care of a patient, the more likely it is that (a) ethics can offer recommendations that impact real clinical options; (b) value-laden conflict has not moved to entrenched positions resulting in immobility; (c) ethics is viewed as a value-added resource to help guide patient care rather than a consult of last resort; and (d) ethical concerns can be adequately discussed rather than a response to situations of clinical crisis.18 Given that the average length of stay for patients with an ICU stay as part of his/her admission to Columbia St. Mary's, adjusted for acuity, is 4.01 days, involvement in the patient's care in less than ten days after admission supports these assumptions.
Table 3
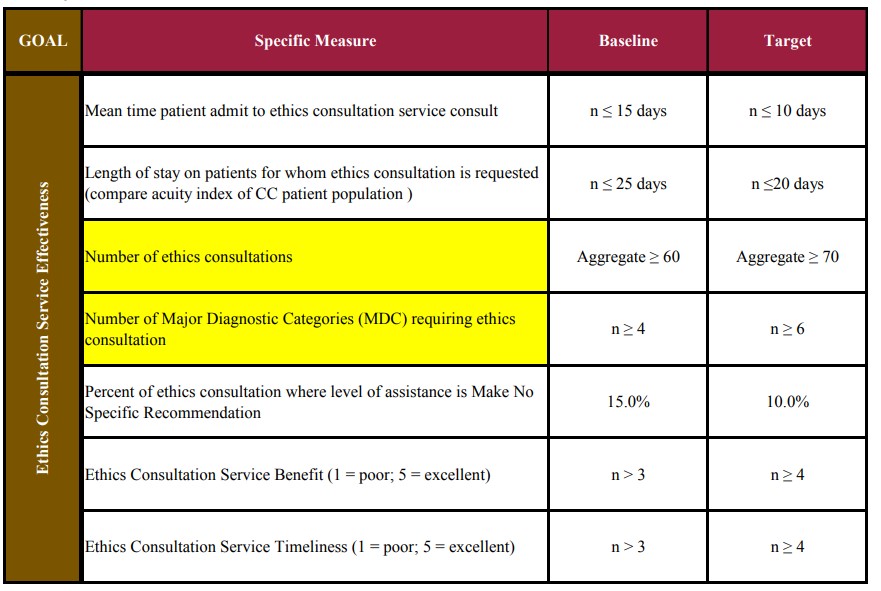
Length of stay (LOS) has been used, most notably by Schneiderman et al. in their 2000 study looking at the impact of proactive ethics consultation in the intensive care setting on timely and consistent decision-making processes.19 Building off this work our dashboard captures LOS but utilizes it for a different measure that contributes to our ethics committee's quality initiatives. Columbia St. Mary's use of the Premier Quality Advisor™ allows our ethics committees to make comparisons regarding the impact ethics consultation has on like acuity patients in the ICU setting.20 Tracking the total number of consultations allows the committee to make year-to-year and month-to-month comparisons on the quantity of consultation to help in asking more critical questions, for example: Why do certain months spike in consultation? Is there any correlation to census? How might we respond institutionally to increasing or decreasing demands for consultation services? Capturing the varying number of Major Diagnostic Categories (MDC) codes for our patient data set demonstrates to the committee and the organization the degree to which we are involved with a clinically diverse set of patients. Again, these data are very helpful in precipitating follow-up questions for ongoing analyses. Two of the remaining three categories for Ethics Consultation Service Effectiveness are self-explanatory, namely, benefit and timeliness. The category that tracks level of consultation requires more explanation, however.
Within the Ethics Tracker database, five levels of consultation are tracked: (a) Recommend a Best Course of Action; (b) Specify a Range of Acceptable Actions; (c) Clarification of CSM Ethics Policy; (d) Retrospective Review; (e) Make No Specific Recommendation — Post-Discharge Review. The last level is arguably the most problematic reason to be consulted. If the patient has already been discharged there is no way that any ethics consultation can have meaningful impact on the hospitalization in which ethical concern was raised. Furthermore, such a consultation request may suggest a more fundamental breakdown in the ethics consultation service itself (i.e., lack of trust, punitive implications of review, etc.). To these ends, our committee has determined that limiting the number of requests where no specific recommendation is desired is a positive quality criterion for the ethics committee and as such should be limited to less than 10% of all requests as a target (Table 3).
Ethics Consultation Service Clinical Collaboration/Integration
The final category is an evolution in thought in an attempt to try to quantify what it means to seamlessly move from clinical ethics consultation to organizational transformation.21 As referenced earlier in this piece, work done by Derenzo, et al. in 2006 demonstrated the benefit of maintaining an active presence of the ethics committee during daily rounds within the hospital. We adopted this literature and integrated an organizational integration metric to track the frequency of rounding in the ICUs as well as with our Family Medicine Residents (Table 4).22 Tracking of continued educational offerings (i.e., Ethics Grand Rounds) and measuring the benefit to the medical staff through the Continuing Medical Education (CME) structure demonstrates the value-added of these services for patient care settings beyond the structure of ethics consultation (Table 4).
Table 4
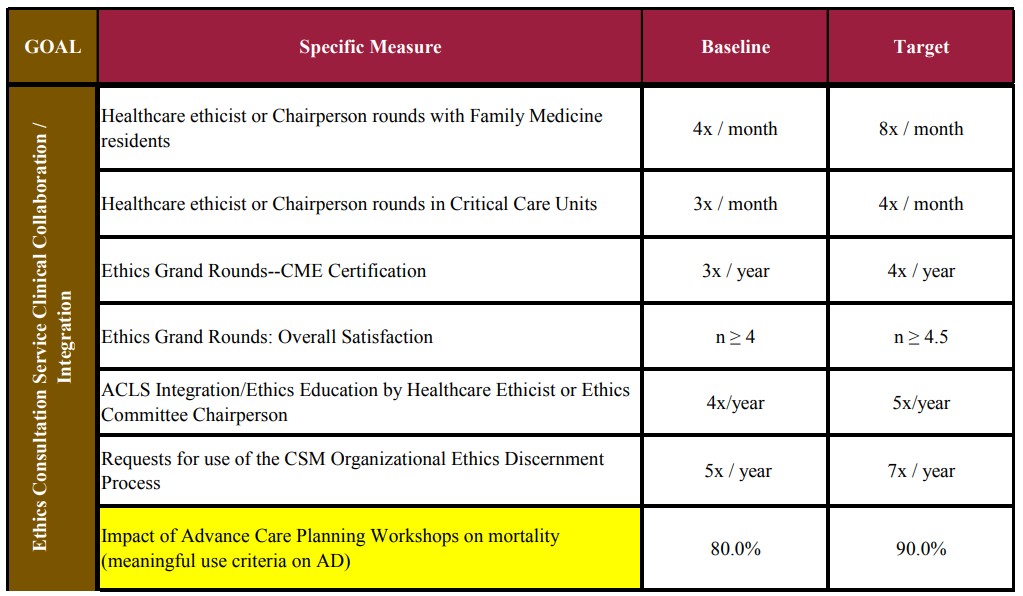
Finally, two measures of clinical integration that correlate highly with the units and issues faced in ethics consultations are ACLS (i.e., ethical issues surrounding code status) and Advance Directive Meaningful Use Criteria (i.e., surrogate decision-making in end-of-life care) (Table 4). Advanced Cardiac Life Support (ACLS) courses through the American Heart Association are offered by certified trainers within Columbia St. Mary's. As part of the curriculum ethics provides a 60-minute training module with an assessment tool on Ethical Issues Associated with ACLS. This case-based module allows for active participation and ethics discourse between ethics committee members and those trained to be involved in code events. Tracking Meaningful Use Criteria (Health Information Technology for Economic and Clinical Health [HITECH]Act) allows for the ethics committee to be fully integrated into quality improvement initiatives around one of the measures medical providers must meet in order to establish that we are using our Electronic Medical Record (EMR) effectively in practice.23 One of the meaningful use criteria is the tracking of documentation related to a patient's Advance Directives. Given our ethics committee's ownership of Columbia St. Mary's initiatives on advance directive education, meaningful use criteria provide an integrated approach for us to measure impact. Clearly, there will be organizational variability with regard to these initiatives, but these examples serve as our ethics committee's metric of active involvement in systemic issues related to quality end-of-life care.
Conclusion
It is no surprise to those in the field of bioethics that we continue to struggle with measuring or quantifying the impact of the work of clinical ethics consultation. It is equally of no surprise that because of that struggle, ethics committees tend to lack the tools necessary to communicate effectively when placed within discussions concerning continuous quality improvement. I would not suggest that the Dashboard template offered in this piece is a substantive display of an understanding of the strategic performance tool known as the Balanced Scorecard.24 But the basis for its design does fall within the ideas laid out in Kaplan and Norton in an attempt to track the impact of ethics consultation on patient care within the categories defined by our professional association as those which comprise the Core Competencies (See Addendum) .
Addendum
By way of example, these data represent the Ethics Dashboard for Columbia St. Mary's from January 1, 2011 through December 31, 2011. Publication of these data has received approval from the CSM Privacy Board. It is to be viewed as an illustration for the benefit of enhancing the points made in this article. Each Table offered throughout this article is a subset of this overall Ethics Dashboard.
- American Society for Bioethics and Humanities. Core Competencies for Health Care Ethics Consultation. (American Society for Bioethics and Humanities: Glenview, IL, 2011).
- M. Repenshek, "A Contribution to the Clinical Ethics Quality Initiative." Internet Journal of Catholic Bioethics 6, no. 1 (Spring 2011), accessed at: http://icbbioethics.com/journals.php?entry=116 (on May 29, 2012); M. Repenshek, "Attempting to Establish Standards in Ethics Consultation for Catholic Health Care: Moving Beyond a Beta Group," Health Care Ethics USA 18, no. 1 (Winter 2010): 5-14; M. Repenshek, "An Empirically-Driven Ethics Consultation Service," Health Care Ethics USA 17, no. 1 (2009): 6-17;
- Glover, J. and W. Nelson, "Innovative Educational Programs: A Necessary First Step toward Improving Quality in Ethics Consultation," In Ethics Consultation, Mark P. Aulisio, Robert M. Arnold, and Stuart J. Younger eds. (Baltimore, MA: The Johns Hopkins Press, 2003): 53-69.
- Glover and Nelson, 53.
- Letter dated November 9, 2009 from the Core Competencies Update Task Force Chairperson inviting ASBH members to contribute to an open comment session on a draft of the Core Competencies for Health Care Ethics Consultation, 2. Accessed at: http://www.asbh.org/uploads/files/pubs/CCUpdateNov09.pdf (June 6, 2012).
- D.J. Opel, D. Brownstein, D.S. Diekema, B.S. Wilfond, and R.A. Pearlman, "Integrating Ethics and Patient Safety: The Role of Clinical Ethics Consultants in Quality Improvement," The Journal of Clinical Ethics 20, no. 3 (Fall 2009): 220-226.
- The Catholic Health Association and Ascension Health. Striving for Excellence in Ethics. (St. Louis, MO: The Catholic Health Association, 2011): 2.
- E. Fox, S. Myers, and R.A. Pearlman, "Ethics Consultation in United States Hospitals: A National Survey," American Journal of Bioethics 7, no. 2 (2007): 13-25.
- ASBH, Core Competencies,
- ASBH, Core Competencies,
- Glover and Nelson, 57-65.
- ASBH, "Core Competencies for Health Care Ethics Consultation." [complete when received].
- D.J. Opel and R.A. Pearlman, "What Is Being Documented in Clinical Ethics Consult Notes? Not Ethics! Poster Presentation, ASBH Annual Meeting, Cleveland, OH, (October 23, 2008).
- K.A. Bramstedt et al., "Optimizing the Documentation Practice of an Ethics Consultation Service," Journal of Medical Ethics 35, no. 1 (2009): 47-50.
- E.G. Nilson et al., "Clinical Ethics and the Quality Initiative: A Pilot Study for the Empirical Evaluation of Ethics Consultation," American Journal of Medical Quality 23, no. 4 (2008): 356-364.
- Solutions (New York, NY: United Hospital Fund of New York, 2004).
- E. Chwag, D.C. Landy, and R.R. Sharp, "Views Regarding the Training of Ethics Consultants: A Survey of Physicians Caring for Patients in ICU," Journal of Medical Ethics 33, no. 6 (2007): 320-324.
- E.G. Derenzo, N. Mokwunye, and J.J. Lynch, "Rounding: How Everyday Ethics Can Invigorate a Hospital's Ethics Committee," HEC Forum 18, no. 4 (2006): 319-31; and W. A. Nelson, W.B. Weeks, and J.M. Campfield, "The Organizational Costs of Ethical Conflicts," Journal of Healthcare Management 53, no. 1 (2008): 41-52.
- L.J. Schneiderman, T. Gilmer and H.D. Teetzel, "Impact of Ethics Consultations in the Intensive Care Setting: A Randomized, Controlled Trial." Critical Care Medicine 28, no. 12 (2000): 3920-3924.
- M. Repenshek, Internet Journal of Catholic Bioethics, accessed at: http://icbbioethics.com/journals.php?entry=116 (on May 29, 2012).
- Letter dated November 9, 2009 from the Core Competencies Update Task Force Chairperson inviting ASBH members to contribute to an open comment session on a draft of the Core Competencies for Health Care Ethics Consultation, 1.
- John Tuohey and Nicholas Kockler, "Ethics Education Enhances Skills of Doctors in Training," Health Progress 93, no. 3 (May-June 2012): 29-37; M. Repenshek and E. O'Tool, "Integrating Ethics into the Residency Model of Physician Education," Health Progress 93, no. 3 (May-June 2012): 34-35.
- See Medicare and Medicaid Electronic Health Record Incentive Programs at http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms/ (Accessed on June 7, 2012).
- R. Kaplan, and D. Norton, "Using the Balanced Scorecard as a Strategic Management System," Harvard Business Review (Jan-Feb 1996): 75-80; R. Kaplan, and D. Norton.. "Transforming the Balanced Scorecard from Performance Measurement to Strategic Management: Part I," Accounting Horizons (March 2001): 87-104; R. Kaplan, and D. Norton, "Transforming the Balanced Scorecard from Performance Measurement to Strategic Management: Part II," Accounting Horizons (June 2001): 147-160.
Copyright © 2012 CHA. Permission granted to CHA-member organizations and Saint Louis University to copy and distribute for educational purposes. For reprint permission, contact Betty Crosby or call (314) 253-3490.