By JULIE MINDA
The United States Conference of Catholic Bishops has developed materials to educate clinicians and others about the practice of female genital mutilation and to guide clinicians in treating these patients with cultural sensitivity and respect.
The resources also are intended to educate women about what to expect when they undergo gynecological and obstetrical care in the U.S. The resources warn of the medical risks related to female genital mutilation, which also is called female circumcision.
The resources are on the CHA website: chausa.org/cutting.
Female genital mutilation is illegal in the U.S. and it is condemned globally as a serious violation of human rights that carries physical and psychological consequences for adolescent girls and women. Because female circumcision is extremely rare in the U.S., medical practitioners encountering a patient who has had the procedure may not know how best to address the patients' needs.
To create the educational and awareness-building materials, USCCB's Migration and Refugee Services partnered with local Catholic Charities resettlement agencies. It engaged with impacted communities to gain a better understanding of the scope of the mutilation practices while also learning more about the impacted women's needs. Through focus groups, a diverse representation of refugee women from all over the world shared stories and concerns about the practice, according to the USCCB.
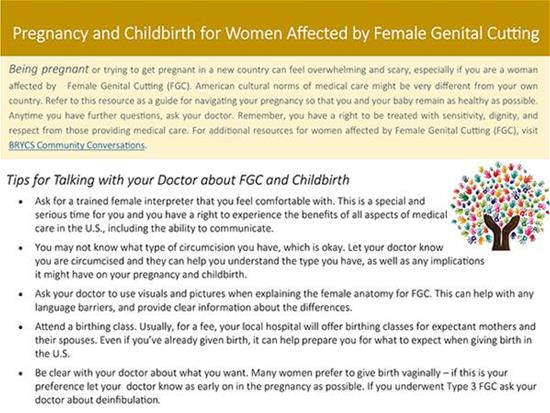
The text above is an excerpt from a brochure to educate women whose anatomy has been altered by genital mutilation. The United States Conference of Catholic Bishops developed this and other patient materials, which are translated in multiple languages, to help women talk to clinicians about their gynecological and obstetrical care. The materials also include fact sheets for clinicians and child welfare professionals.
The materials published by the bishops' conference include fact sheets on mutilation for health care practitioners and child welfare professionals and health information for women who have undergone genital cutting.
The materials explain forms and degrees of female genital mutilation.
The resources for clinicians describe the potential health risks associated with genital mutilation and explain how to approach the subject with patients in a culturally sensitive manner. Patients may be unfamiliar with their own anatomy and come from cultures where gynecological and prenatal care are not the norm.
The materials for patients explain how their altered anatomy may impact their gynecological health, including during pregnancy, delivery and postpartum.
USCCB's Migration and Refugee Services office created the materials under their Bridging Refugee Youth and Children's Services program, which aims to strengthen the capacity of refugee-serving and mainstream organizations across the U.S.
The U.S. Department of Health & Human Services' Office on Women's Health provided grant funding for the USCCB's awareness-building and education around female genital mutilation. Although health care providers and their patients are the primary audience, the materials also are aimed at child welfare professionals, educators and immigrant communities where female circumcision may be practiced.
According to the World Health Organization, female genital cutting has been documented in 30 countries, mainly in Africa, the Middle East and Asia. It is performed for a variety of cultural, religious and other nontherapeutic reasons. It is usually done before girls are age 15. Materials from the USCCB suggest that clinicians ask their adult patients who have undergone female circumcision whether they intend to have their daughters undergo the ritual, and that the clinicians explain the health implications of the practice.
Information from WHO indicates the degree of mutilation correlates with the potential adverse health consequences for women, especially during pregnancy, delivery and the postpartum period.
Women who have been mutilated can be at heightened risk for wound infections and hemorrhaging during delivery. Their infants may be at higher risk for intrauterine death or lifelong adverse health consequences.
WHO says about 200 million girls and women alive today have undergone genital mutilation. The USCCB materials say an estimated 513,000 girls under age 18 in the U.S. have experienced or are at risk of mutilation.
Immigrants to the U.S. who are part of cultures that practice genital cutting may be unaccustomed to talking about gynecological matters or accessing gynecological services. The USCCB resources say it is important that clinicians be sensitive to patients' fears and discomfort in broaching the subject with a medical professional. The materials say patients may feel more comfortable with a female physician and recommend that clinicians involve female interpreters in these patients' care when appropriate. Conversations with patients should be respectful and protect patients' dignity.
Clinicians should clearly describe services before providing them, use visual aids when describing gynecological terms and procedures, and take extra time to explain the potential consequences of medical options. The resources explain how to approach especially sensitive topics such as advising women whose cutting was reversed for a delivery, but who wish to restore the cutting postdelivery.