Many ethical considerations have arisen regarding the development and distribution of vaccines for COVID-19. Catholic Health World Associate Editor Lisa Eisenhauer asked Jason Eberl, a professor of health care ethics and director of the Albert Gnaegi Center for Health Care Ethics at Saint Louis University, for his perspective on some of those issues.

Eberl
What are your thoughts on the recommendations to the Centers for Disease Control and Prevention from its Advisory Committee on Immunization Practices that frontline health care workers and residents and staff at long-term care centers should be the first to get the COVID-19 vaccine?
It seems logical to me to prioritize health care workers, those in essential positions. When you're dealing with a public health crisis, there is a relevant principle, the common good, to focus first on those who, if they are to get sick and are unable to work, would have a multiplier effect on care for others. We all benefit from those who care for us being protected first, plus there is an argument that we owe it to them as reciprocity for having put their health and lives on the line for us.
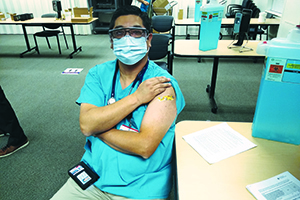
Dr. George Diaz, section chief, infectious diseases at Providence Regional Medical Center in Everett, Washington, shows the bandage on his arm where he got his COVID-19 vaccine injection. Diaz was the first doctor to treat a patient confirmed to have COVID in the United States and the first doctor in the world to administer the antiviral drug remdesivir. The hospital is part of Providence St. Joseph Health.
What do you see as the major ethical issues related to any COVID vaccine?
If we're talking about any vaccine in general, of course, one of the first issues from a Catholic perspective is: Was the vaccine developed in an ethical manner? There are some vaccines that are built using cell lines that were developed about 40 years ago from tissue from aborted fetuses. Back in 2005, the Congregation for the Doctrine of the Faith issued a statement (reaffirmed in the 2008 document "Dignitas Personae") basically stipulating that while it's unethical to develop vaccines from those cell lines, it is permissible for people, if they have no other alternative vaccine available to them, to utilize that vaccine.
Thankfully, the Pfizer and Moderna vaccines do not have this ethical issue. The AstraZeneca one does, but the Congregation for the Doctrine of the Faith has just affirmed the previous teaching allowing for Catholics in good conscience to be vaccinated by any of the available vaccines, even if they were produced through immoral means.
Any other issues?
The next major issue has been about making sure that we are adhering to principles of a just, equitable distribution of resources. CHA has published ethical guidelines in this regard, calling, first of all, for demonstrating the safety and efficacy of the vaccines, and then assuring that the decisions on prioritized distribution of vaccine are consistent with Catholic social principles including the dignity of the human person, the common good, subsidiarity and the preferential option for vulnerable persons. When you look at the common good and the preferential options for vulnerable persons, what the CDC has recommended makes sense to me, including the most recent call for those over 75 years of age and frontline workers in essential industries to be vaccinated in the next round.
Does the U.S. have a duty to ensure people without legal immigration status in the U.S. have access to the vaccine?
I don't think prioritizing citizens over noncitizens is ethically justifiable since there is no principle of Catholic social teaching that justifies this form of discrimination. Plus, if one looks at it from a pragmatic perspective, then ensuring maximal vaccination makes sense, because it protects all of us in the end.
COVID has hit communities of color especially hard, and those communities have been the victims of poor care and maltreatment by the American health care system. Is there justification for people in communities that suffered inequities in care to be suspicious about getting a vaccine?
Given the history of egregious unethical treatment of people of color in the U.S. by the medical community, including the infamous Tuskegee syphilis study by the U.S. Public Health Service, I think there is a historical basis to justify distrust. But, looking at the present day, while there's still a great deal of health disparities experienced by various minority groups, people of color in particular, we have very robust research regulations that are specifically in place to protect exploitation of members of these groups again. From what I've seen in terms of how they have enrolled people in the vaccine studies — there were over 40,000 people in the case of the Pfizer study — there was no exploitation happening. Therefore assuming adequate review by the Food and Drug Administration, I don't think that that history justifies the present attitude of distrust about this particular vaccine.
Does the U.S. have a special duty to build trust among vaccine sceptics in communities of color?
Yes, through education. Honest information, transparency, going out to local communities, talking with local church groups and so on, I think, is imperative to educate people, especially when there's so much misinformation being put out through the internet, through disreputable media sources.
What is our responsibility to people in prisons and jails with respect to vaccine distribution?
The incarcerated have as equal a right as those of us who have not been convicted of a crime to receive access to the vaccine.
Do we as a nation have a responsibility to share any vaccines that we develop with poorer nations that don't have the same resources?
Absolutely. Pope Francis, in his recent book Let Us Dream and elsewhere, has called on us to adopt a global perspective, recognizing that we are all brothers and sisters in Christ, baptized or not, whatever country we live in. The preferential option for the poor and vulnerable extends beyond any national borders. And, from a purely pragmatic perspective, people travel, and part of the reason the virus spread so quickly is major global travel. If we want to resume that level of global travel then it is in everyone's best interest to share the vaccine.