Trust building, authenticity are essential
By JULIE MINDA
People of color have had higher rates of infection, more severe illness and higher rates of death from COVID-19 than white people. Many in the health system in the U.S. are aiming to ensure people in minority populations get equitable access to vaccination. Vaccine hesitancy is an early hurdle they are working to surmount.
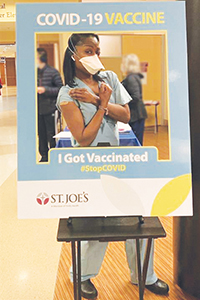
Thoracic surgeon Dr. Kumari Adams of Saint Joseph Mercy Health System of Canton, Michigan, mugs for the camera after receiving a COVID inoculation.
In a survey conducted by the Pew Research Center in late November before regulators gave emergency approval to the first vaccines, 42% of Black and 63% of Hispanic adult respondents said they would definitely or probably get immunized as compared with 61% of white adults. About 18% of the total survey group said that although they didn't want to be among the first groups to be vaccinated, they hadn't ruled out being vaccinated.

Robinson
A sampling of Catholic health leaders said their systems and facilities are committed to addressing racial disparities as part of the national COVID vaccination effort. They are being intentional about listening to the concerns of members of the public who are worried about vaccination and then addressing those concerns. The systems are focusing outreach efforts on minority and other vulnerable populations, including Black and Hispanic people and immigrants.
Dr. Loren Robinson, vice president of medical affairs at CHRISTUS Health, said it is central to the ministry's mission to "keep people in the communities we serve healthy and out of the hospital so they can live their best and healthiest lives." Robinson said to do this, the ministry "must address the long and storied history" between people of color and the health system.

Capeles
"We need to be transparent and accurate — we're here as a resource. That is our duty," said Tiffany Capeles, CHRISTUS system director, health equity, diversity and inclusion.

Medows
'Tragic impact'
Dr. Rhonda Medows is president of population health management for Providence St. Joseph Health and chair-elect of CHA's board. She said for many, vaccine hesitancy is rooted in "the disproportionate and tragic impact of health disparities on people of color — including Black, Latino, Native and indigenous peoples." She said many of these populations have a long history of suffering immoral and inhumane treatment at the hands of medical professionals, including being the unwitting subjects of cruel and dehumanizing medical experimentation.

Slubowski
Mike Slubowski, president and chief executive of Trinity Health, said that while the most egregious cruelties are in the past, data shows that disparity continues today, including conscious and implicit bias in the care that is delivered to people of color.

Laird
Shivonne Laird, Bon Secours Mercy Health's director of community health impact, added that compounding such inequities is the fact that, as a group, people of color can be at higher risk of contracting COVID and fare worse under COVID in part because of social determinants.
For instance, a recent study found that many Black and Hispanic families are more likely to live in multigenerational households and hold essential jobs that can't be done from home, increasing their COVID risk.
Medows said, "We need to acknowledge what has happened in the past and what is happening now and respect people's realities. But we are saying to not let past history stop us from doing what we can to get us beyond this pandemic."
Role models
Slubowski said Trinity Health is using the system's 123,000 colleagues across 22 states as a type of microcosm for the population at large. The perceptions they've shared are consistent with national polling conducted by others: employees who are people of color have expressed more concern than their Caucasian colleagues about vaccination. Part of how Trinity Health has been addressing such hesitancy is by engaging its clinical and administrative leaders who are minorities in talking to employees about their confidence in the COVID vaccines.

Dr. Norvell Coots, president and chief executive of Holy Cross Health in Silver Spring, Maryland, and chief executive of Trinity Health's Maryland region, celebrates with colleagues after receiving his COVID vaccination. Coots, who is Black, has been encouraging people of color to get vaccinated.
CommonSpirit Health says it is encouraging employees to get vaccinated through outreach that includes debunking myths about vaccine danger. To spread the word about vaccine safety to hard-to-reach communities, employees of color are posting vaccination selfies on their social media accounts. Many facilities have stood up "selfie stations" for this purpose.
Employees can play a powerful role in encouraging others to get the COVID vaccine, especially in vulnerable populations, CommonSpirit said in a press release. Employee survey re–sults released in late January showed 69% of Black respondents and 77% of Hispanic respondents said they have been or intend to be vaccinated.
Community connections
Trinity Health and Providence St. Joseph Health are tapping into the informal and formal networks of community health workers that they had been establishing well before the pandemic began. These individuals promote the health of their neighbors and improve health care access for medically underserved people. Their close ties to the community are proving vital now.
The community health workers are listening posts for the health systems, meeting with community and church groups and their own clients to get unfiltered information about the reasons behind vaccine hesitancy or barriers to vaccine access and reporting back to their health systems. They're also engaging with other community influencers to spread their pro-vaccine public health message.
Laird said the community health leads in each Bon Secours Mercy Health market are helping planners understand how language barriers, mistrust of the health system and government, lack of broadband access among rural community members and similar issues may be contributing to vaccine hesitancy in these communities. They're strategizing with the planners on ways to overcome the barriers. Bon Secours Mercy Health operates in seven states.
Robinson and Capeles said an equity task force at the four-state CHRISTUS is spearheading similar intelligence gathering.
Avera Health is working with individuals who hold sway in immigrant communities and representatives of organizations that are intertwined with these immigrant communities on vaccine acceptance. Such influential community members had smoothed COVID screening and testing efforts early in the pandemic, around the time that hotspots were first occurring in South Dakota. These community leaders helped Avera gain the trust of undocumented immigrants wary of health care workers. Those same people now are helping Avera understand immigrants' concerns about vaccination.
Bidirectional communication
Catholic health systems have been using the intelligence they are gathering on the ground and on social media to tailor their vaccine education and outreach to minority and other vulnerable communities.
Medows regularly scans and posts on TikTok, Facebook, Linked In and Twitter to monitor public perception of the vaccines. She's seen deceptive posts declaring that the vaccines contain microchips for tracking recipients. Another myth is that the vaccine will be used to sterilize women of color.
Ministry systems and hospitals are hosting virtual town halls and webinars; encouraging their clinicians who are people of color to speak — in person or virtually — before churches and community groups; creating videos of people of color attesting to the efficacy of the vaccine; and rolling out social media campaigns to share information about vaccine safety, efficacy and access.
Slubowski of Trinity Health noted that an ongoing challenge is balancing the great need to build confidence in the vaccines with the need to encourage patience, since most members of the public are having trouble accessing the vaccines currently, due to distribution issues.
Authentic voice
Laird said system and facility spokespeople are being honest about not having all the answers about the vaccines. Bon Secours Mercy Health representatives are working with community partners to understand what information would be helpful and the best ways to share this information. Bon Secours Mercy Health associates coordinating communications about vaccination are being careful to ensure that their efforts to put forward spokespeople are authentic. "We wouldn't just want to spotlight a person of color, for example. We would want people to be able to see themselves and their values reflected in the message shared," she said.
Medows noted Providence St. Joseph Health takes pains to make sure people who are concerned about vaccines are treated with respect. "If we minimize people's concerns, we lose the ability to communicate with them."
Robinson said CHRISTUS is ensuring that its vaccine education efforts are not perceived as pressuring people to take the vaccine. "Instead, we are empowering people with information to make decisions," she said. Capeles added that honest, two-way communication with people of color "can build a bridge and cultivate trust."
Slubowski said of Trinity Health, "We take our role as a trusted health partner seriously. We believe the vaccine is the best path for ending this pandemic, and we are 100% confident in the vaccine. We're using every vehicle we can to convey that to people."
Trinity Health executive overcomes vaccine hesitation
SSM uses data to prioritize vulnerable people for inoculation
Like countless other health care providers across the U.S., St. Louis-based SSM Health is coordinating a massive vaccination effort involving its own employees and patients as well as emergency workers and members of the public. As part of that process, it is aiming to ensure that vulnerable populations that have been overlooked or marginalized in public health efforts of the past, receive equitable treatment this time around.
One way SSM Health is doing this is by using data collection and analytics to help ensure that people at risk of marginalization are instead prioritized for inoculation, according to Dr. Michael Scharff, regional chief medical information officer for SSM Health's Greater Midwest Region.
SSM Health is part of a regional collaboration of health care systems and facilities that have been coordinating their response to the pandemic and that are now working together to vaccinate as many people in the region as efficiently as possible, given limited resources. They are adhering to state protocols on tiering vulnerable populations. As of early February, they had inoculated most of their eligible hospital and long-term care employees as well as first responders, emergency services personnel and public health workers. And, they had just begun inoculating individuals the state defines as high-risk including people over the age of 65 and people with serious underlying health conditions. .
For the inoculation of high-risk individuals, SSM and the other health systems in the collaborative are starting with patients of the practices within their own systems, according to Scharff. The systems are contacting their patients in age-based stair steps, starting with those age 85 and over to offer an inoculation appointment, followed by those 75 and up, and then those age 65 and up, he said.
Scharff said during this phase, SSM also is using data analysis to identify its patients that have the most pronounced need in terms of social determinants of health, and it is offering vaccination appointments to those at critical risk according to their level of socioeconomic need.
SSM also is aiming to identify vulnerable people for prioritization, among members of the general public. It has an "interest form" on its website that people can fill out to indicate that they wish to be vaccinated. Among other questions, the form asks: "Are you in a racial/ethnic minority group that has been disproportionately affected by COVID? (e.g.: African American; Indigenous; Latino; Hispanic)"
Scharff said SSM is retaining the data submitted through the forms on lists that it will use for scheduling vaccination appointments, both for people who are SSM patients and people who are not. It will conduct this outreach once it has finished vaccinating the people identified in high-risk categories among its own patients. As it moves through the list of people who filled out the interest form, it will prioritize those who are elderly and those who answered "yes" to the question about being in a racial or ethnic group disproportionately affected by COVID. Scharff said the prioritization is done algorithmically.
He added, "As a whole, SSM is very mindful of the populations we are serving, and we are very mindful that we are here to serve the population as a whole. This type of prioritization helps us focus on those we may not have been as attentive to in the past. We need to ensure we're giving them equitable care."
He noted that SSM is aware that many people who are in vulnerable populations may not be technologically adept or have access the online entry points that SSM and other health care providers have created to get in line for vaccination. Scharff said SSM and others on the regional task force are looking at how to use word of mouth and other nontechnical methods of making people aware of how to get in line for vaccination, without online access.