By LISA EISENHAUER
In January, Loyola Medicine opened a specialty neurology clinic that amounts to a stake in the ground on what could be the next frontier of the COVID-19 pandemic. It treats patients struggling with debilitating and unrelenting symptoms weeks or months after the acute stage of the infection.
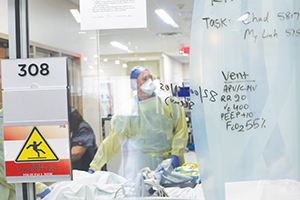
A care provider treats a patient with a history of COVID-19 in an intensive care unit at SSM Health DePaul Hospital in suburban St. Louis. Early studies show that about 10% of people who are infected with the virus suffer long-term symptoms, such as fatigue, headaches and sleep disturbances. Lisa Eisenhauer/© CHA
The condition known as long-haul COVID or long COVID is thought to occur in about 10% of people infected. It may reflect persistent immune activation and/or lingering inflammation, and may be independent of the severity of the initial COVID infection.
Dr. José Biller, professor and chair of the department of neurology at Loyola University Medical Center in suburban Chicago and Loyola University Chicago Stritch School of Medicine, heads the clinic with two neurology colleagues. While the clinic's focus is on neurological manifestations, the doctors will refer patients to other collaborating specialists — including psychiatrists, neuropsychologists, pulmonologists, cardiologists, nephrologists, gastroenterologists, physical therapists and nutritionists — as needed.

Biller
Biller said that even though research on long-haul COVID is in the earliest stages, evidence that the infection can leave patients with lingering health problems is clear.
Biller and his colleagues at Loyola Medicine — a three-hospital system that is part of Trinity Health — are evaluating and managing patients who are weeks past the acute stage when the virus was detectable in their systems, yet still ailing. The patients' symptoms may include severe fatigue; brain fog; loss of smell (anosmia); a distorted sense of taste or inability to taste (dysgeusia); headaches; vertigo; sleep disturbances; loss of muscle mass and strength (sarcopenia); and autonomic nervous system dysfunction, muscle cramps and pain (myalgia).
Biller pointed to the results of a survey of 3,762 post-COVID patients from 56 countries that was published in late December on the medical research website medRxiv. The patients described more than 200 different symptoms, the most common of which were fatigue, post-exertional malaise and cognitive dysfunction.

A clinician at Loyola University Medical Center in suburban Chicago prepares to enter the room of a patient being treated for COVID-19. The medical center has treated more than 1,000 patients who have contracted the virus in the past year.
"What we know already about the condition, even though our knowledge is really less than one year old, based on what we have seen at Loyola and what the literature states, is that about two-thirds of individuals who have had long-haul COVID may not be able to return to full health," Biller said.
Whether those patients will eventually regain their full health remains to be seen, he said.
Estimates of how many patients go on to develop long COVID syndrome vary widely. Even the definition of the malady is in flux. A paper published in The BMJ in August said long COVID appears to be a multisystem disease. Symptoms run along a continuum from burdensome to deadly. The condition can occur after a life-threatening or relatively mild case of COVID. The researchers defined long COVID, or chronic COVID, as symptoms that last for at least 12 weeks beyond the onset of the virus.
In May, Mount Sinai Health System launched what it called the "first-of-its-kind" Center for Post-COVID Care to offer treatment from a multi–disciplinary team of specialists. The system did not define its target patient population beyond those who need COVID-related aftercare.
Stricken on the job
One of Biller's patients is a woman in her 50s who was exposed to the virus on the job and tested positive in August. She had no underlying conditions to put her at elevated risk and she nursed the virus at home under the supervision of her primary care doctor. (See sidebar.) Despite some lingering symptoms like headaches and fatigue, she was well enough to return to work in October.
By the end of the year her employer had notified her of three more exposures — the second and third exposures within two days of each other — and she went into quarantine each time. She had only one bout with acute illness.
She hasn't returned to work since late December when she was struck with speech problems so serious that she went to an emergency room two days in a row. A month later, her voice remained uneven. "My voice goes good for a while and then it goes bad. I get high volume, low volume. I get everything," said the woman, who spoke on the condition that she not be identified.
"The biggest rumor and myth is that people believe you have preexisting conditions" to have bad outcomes, the woman said. "I had nothing."
Steen
Heart afflictions
Dr. Lowell Steen is an interventional cardiologist, chief of cardiology for Loyola Medicine and a professor of medicine at Loyola University. He said his care of COVID patients and review of research confirms that those with long-term symptoms are not necessarily those who had health issues beforehand or those who suffer the severest cases of the infection.
He pointed to research published in July by JAMA Network. Doctors in Germany studied 100 recently recovered COVID patients who all underwent cardiovascular magnetic resonance imaging. "A total of 78 patients who recovered from COVID-19 infection had cardiovascular involvement as detected by standardized CMR, irrespective of preexisting conditions, the severity and overall course of the COVID-19 presentation, the time from the original diagnosis, or the presence of cardiac symptoms," the study found. Two-thirds of the patients in the study had not been hospitalized for COVID.
"I think the messaging about COVID early was not everyone's going to die from it, it's only 1%," Steen said. "But my message to people is you don't want to get COVID because we just don't know the long term on it. And this is a perfect example of what I'm talking about, which is that even though you may tolerate the infection fine and think you're fine, there are some long-term effects that you may not be aware of."
The most prevalent problem the German study discovered was inflammation, which Steen said parallels what he and his colleagues have seen at Loyola. They even have had acute COVID patients present with symptoms that would indicate a major heart attack only to have testing reveal no blockage, pointing to inflammation as the culprit.
While the link between COVID and heart complications is in the early phases of study, Steen said it's another reason the virus should not be taken lightly even by people who are in top condition. He said he worries about professional athletes who resume playing just days after their COVID recovery. He recommends that his patients wait six weeks after they are cleared of the virus before they return to intense exercise.
"We think COVID's primarily an illness of the lungs because that's where all the ACE2 receptors (that the virus binds to) are, but we now have scientific evidence that that's not (exclusively) true," Steen said. "It's not just the lungs, it affects the heart as well, so we have to be mindful of that."

Larned
Many unknowns
Dr. Joshua Larned is a cardiologist and medical director for congestive heart failure services at Holy Cross Health, a teaching hospital in Fort Lauderdale, Florida, that is also part of Trinity Health. He and colleagues there are conceptualizing a cross-disciplinary care program for post-COVID patients who have long-term symptoms.
"We're starting to see patients who are recovered from COVID, a large amount of them, who have some form of ongoing medical issue that they didn't have before their COVID illness," Larned said. How long the patients' symptoms will last and whether those symptoms will affect their life spans are questions "we simply don't have an answer to yet," he said.
Another unknown that concerns Larned is how prevalent the conditions are because many post-COVID patients and primary care doctors might not have made the connection between lingering symptoms and the infection. Until that is determined, he said the medical system won't know how taxing caring for these patients is going to be.
"This is a very, very important topic," Larned said. "The story needs to be told now because we're focusing so much of our effort appropriately on prevention and vaccination and managing COVID illness in its acute phase, but we haven't really wrapped our clinical expertise around some of these symptoms that are present in the recovery phase."

Carlson
Another reason for vigilance
Dr. Ethan W. Carlson is a family practitioner in Baraboo, Wisconsin, and medical informatics director for SSM Health in Wisconsin. He said he and his colleagues are seeing many patients with what could be long COVID. They have symptoms like fatigue, loss of taste or smell, coughs and gastrointestinal issues that won't go away.
As to whether their ailments are definitely connected to COVID, Carlson said: "Of course we do not know that, and we cannot say that."
While doctors and patients wait for researchers to confirm the link and devise the best treatment protocols, Carlson is doubling down on his efforts to get his patients to take all precautions to avoid contracting COVID.
"I think for quite some time we're going to have to reinforce the importance of masking and social distancing and all the behaviors that have been important at the beginning and middle of the pandemic," he said.
Infection strikes patient in peak health, leaves lingering challenges
She wowed her colleagues in July when she did a handstand on the armrests of a seat. It was a demonstration of strength and agility the 56-year-old had honed over years as a gymnast and later as a coach.
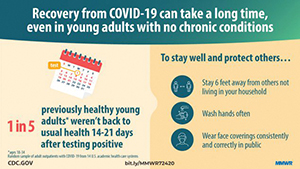
An explanatory graphic from the Centers for Disease Control and Prevention warns of long-term effects from COVID-19.
She regularly swam 40 laps and bicycled for 10-15 miles. These days, just getting dressed can leave her winded.
The woman, who spoke on the condition that her name and line of work not be revealed, said her athletic prowess drained away after she came down with COVID-19 in August. She joined a growing group of patients who endure lingering symptoms. Hers are uncontrollable fluctuations in the volume and timbre of her voice, severe headaches, shortness of breath and memory loss.
She weathered the acute stage of COVID alone at her suburban Chicago home. She felt miserable, but her six siblings took turns checking on her and dropping off medicine and groceries. She had virtual visits with her physician and used a pulse oximeter to monitor her blood oxygen level.
After her recovery she was cleared to return to work in October. On her first day back, she was exposed to the virus again. While quarantining, she studied for an annual exam required to keep her job. Severe headaches and a general brain fog made her feel almost as if she had suffered a concussion. "I was so nervous and had to study so much extra on subjects that should be easy for me from years of training," she recalled. She did pass the exam.
While back on the job in December, she was exposed to COVID twice more. She has since been recuperating at home while she deals with her lingering symptoms and the new one that arose at the end of December: the inability to modulate her voice. Tests confirmed that she hadn't had a stroke and she was negative for COVID.
Since then, she has been under the care of Dr. José Biller, chair of the department of neurology at Loyola University Medical Center. By mid-January, he had ruled out aphasia, a loss of ability to understand or express speech caused by brain damage. More evaluations are under way.
Meanwhile, she is working to overcome exhaustion and rebuild her endurance. Tests show that her heart and lungs are healthy.
"I get tired every day of everyone asking me how I am," she said. "I know they mean well but I get tired of thinking about it because I want to stay positive and focused."
— LISA EISENHAUER