By JULIE MINDA
As a bedside nurse, Vernette Townsend has held the hands of transplant candidates as they learned that they had been matched to a donor organ and she's cared for patients who would die waiting for an organ. "I will never forget those moments," she says.

Townsend
Now, as chief nursing officer for Trinity Health Of New England's Saint Francis Hospital, that experience motivates her as she works to build awareness of the profound impact of organ donation and the particular need to increase the number of donated
organs. This includes convincing more Blacks, Hispanics, Native Americans and Pacific Islanders to register as potential organ donors. Townsend educates audiences about organ donation at churches in the Black community.
People of color have higher rates of diabetes and high blood pressure than whites, a propensity the National Institute of Diabetes and Digestive and Kidney Diseases says puts them at higher risk for organ failure. Members of these minority groups
are overrepresented on transplant waiting lists and underrepresented among donors. African Americans have the proportionately highest need for organ transplant of
all minority groups in the U.S., according to the Department of Health and Human Services Office of Minority Health.
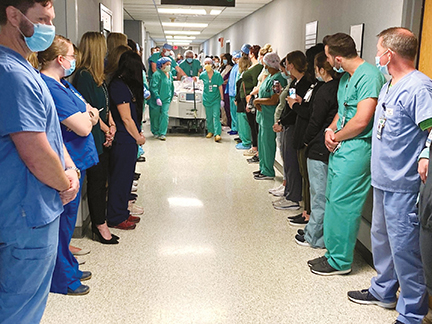
Clinicians stand in silent tribute as an organ donor's body is transported to a surgical suite for the organ removal. The March 2021 "hero walk" took place at St. Francis Medical Center in Monroe, Louisiana, part of Franciscan Missionaries of
Our Lady Health System.
There are multiple factors that go into matching a donated organ with a transplant candidate, including medical urgency and the most efficient use of the organ. Donors and transplant candidates of different races frequently match on organ donation.
According to the Health Resources & Services Administration, shared race or ethnicity is not a requirement for successful organ donation, but in rare cases it can determine whether a match is made.
Transplantation is more apt to be successful between donors and recipients with similar immune cell markers. Since immune system markers are inherited, HRSA says having a diverse donor registry increases the chance of finding a good match for transplant
candidates. Donate Life America, a nonprofit that promotes organ donation, says shared genetic background may increase the chance of longer-term survival posttransplant.
HRSA says tissue-type matches central to the success of bone marrow or cord blood transplants are most likely among people of the same race and ethnicity.
The agency is working to increase marrow and cord blood donations from Native Americans, Blacks, Hispanics, Asians and Pacific Islanders.
Some Catholic hospitals are doing their part to encourage members of minority populations to register as organ donors. Some of the campaigns are built around National Minority Donor Awareness Month, which originated in 1996 and runs through August.
Donor disparity
Donate Life America says there are more than 100,000 people waiting
for transplants in the U.S., and nearly 60% of them are minorities. The Department of Health and Human Services Office of Minority Health says that 28.5% of candidates awaiting a transplant are Black; 12.9% of organ donors are Black. There are similar imbalances for other minority populations.
Franciscan Missionaries of Our Lady Health System in Louisiana; Hospital Sisters Health System's Wisconsin regions; St. Joseph's Health in Paterson, New Jersey; and Trinity Health Of New England have workgroups coming up with ways to increase organ
and tissue donations among all potential donor groups, with special attention to minority populations. The health systems commonly collaborate on these efforts with their local organ procurement organizations.
All these systems have hospitals engaging in community outreach throughout the year to educate and dispel misinformation. They employ traditional and social media channels. When possible, they dispatch representatives, who have a similar cultural,
racial or ethnic background as the intended audience, to churches, community events, community organizations, schools, barbershops and other venues.

Brevard
Mark Brevard directs multicultural community outreach for New England Donor Services, the organ procurement partner of Trinity Health's Saint Francis Hospital in Hartford, Connecticut. He says his organization is being intentional in hiring representatives
from diverse backgrounds to better reflect the demographics of the families with whom they are speaking about the opportunity for donation.
They attempt to normalize conversations about organ donation.
HSHS' Western Wisconsin region has organ donation experts staff a booth at community baseball games and hand out information at family movie events.

Averhart
Steven Averhart, director of family services for New England Donor Services, says awareness-building and education are intended to get people thinking of organ donation — and signing on as donors — well before a critical life event.

Aidt
Tammi Aidt is manager of supportive care services for FMOLHS' Our Lady of the Lake Regional Medical Center, Baton Rouge, Louisiana. She says FMOLHS and the organ procurement organization it works with do outreach and education in neighborhoods
with concentrations of minority residents for the same reason — to start conversations when there is time for calm discernment.
Our Lady of the Lake hosts community events that highlight the altruism of organ donors and their families. It puts donors' names on its Silent Hero Wall and each April during Donate Life Month it invites the public to its drive-thru Path of Remembrance,
where donors are honored with tribute signs and a butterfly release.
Generational divide
Anne Pretasky, nurse manager and director of critical care services at HSHS Sacred Heart Hospital, Eau Claire, and nurse manager of HSHS St. Joseph's Hospital — Chippewa Falls, says a lack of cultural
familiarity lowers the comfort level and keeps organ donation rates relatively low among Hispanic, Native American and Hmong communities in her hospitals' catchment areas.
She adds that older adults in these minority groups may be more uncomfortable with the concept of organ donation than their children and adult grandchildren.

Chowdhury
Tanwir Chowdhury is director of nursing for critical care at St. Joseph's in Paterson, which covers a diverse population and so directs much of its organ donation education efforts at minorities. Chowdhury says some individuals decline to check
the organ donor box on their driver's license because they believe that medical professionals will not try as hard to save the lives of people who are organ donors. Organizations that procure or transplant organs call this supposition a myth
and work to debunk it.

St. Joseph's Health and its organ procurement partner hold a flag-raising ceremony at St. Joseph's University Medical Center in Paterson, New Jersey, to mark National Donate Life Month in April. From left are Ryan Smith, clinical donation
specialist, NJ Sharing Network; Veronica Myers, hospital services manager, NJ Sharing Network; Kevin Slavin, president and chief executive, St. Joseph's Health; Todd Brower, senior vice president and general counsel, St. Joseph's Health;
and Tanwir Chowdhury, director of critical care nursing at St. Joseph's Health.
When a patient being kept alive on life support has not indicated a willingness to be an organ donor by checking a box on their driver's license, a spouse or family member with legal decision-making authority ordinarily is asked to make the organ
donation decision.
Families of patients who are people of color are less likely than white families to agree to organ donation, Chowdhury says. He says those who decline often cite cultural or religious aversions to organ donation, though he says such concerns are
not unique to people of color.
Saint Francis' Townsend says the historical mistreatment of Blacks by the medical system factors into the reticence about organ donation.
Averhart observes that some people of color choose not to register as organ donors because they believe minority people are deprioritized as recipients.
There is evidence that has been a defacto result of a method of evaluating the severity of kidney disease used to rank order people awaiting transplants. In June, the board of directors of the Organ Procurement and Transplantation Network sought
a remedy, eliminating an assessment criterion that led "to a systemic underestimation of kidney disease severity for many Black patients."
Education first
The ministry and donor procurement executives say recruiting more members of minority populations to become potential organ donors requires establishing trust and building a hospital culture that routinely
promotes organ donation.
All the ministry executives say their facilities work with their procurement organization partners to educate hospital staff on the practical and emotional aspects of organ donation for donors' families. The staff of hospitals where donations
are made are the first line in building trust with families. In many hospitals staff demonstrate sincere reverence and honor for donors and their families by lining up in halls in silent tribute to the donor as his or her body is wheeled to
the surgery suite where the organs will be harvested.
The executives say there has been a slow increase over time in organ donation, including among minority populations. But, they say, much work remains.
HSHS' Pretasky says, "We want to maximize the number who say yes to organ donation, and we look at every possible way to maximize that number. But it really comes down to developing great relationships with family members. Patients and families
have a real connection with our staff, and those workers share themselves to make a connection on a human level," and that is what makes a difference.
Hospitals, organ procurement organizations partner to broach organ donation with families
Fewer than 1% of people die in a way that allows for organ donation, says the United Network for Organ Sharing. In most cases,
candidates for organ donation are patients on life support in intensive care units who are being assessed medically to determine whether they are brain dead. Their deaths may have been sudden and unexpected, the result of an accident,
an assault, an aneurism or heart attack.
It is usual in these circumstances for a family member with legal decision-making authority to authorize organ and/or tissue donation, even when a patient has given their consent to become a donor in advance through a driver's license
registration process or other means.
Ethicists say it is incumbent on hospitals and the organ procurement organizations they partner with to ensure these consent conversations with immediate family members are handled delicately and with empathy, respect and compassion.
"The relationship-building and trust is established between the hospital staff and patient's family from the moment they enter the hospital through the ER," says Vernette Townsend, chief nursing officer for Trinity Health Of New England's
Saint Francis Hospital. "Families need to feel heard, seen and recognized to trust in the care and treatment by hospital staff for their loved ones. Continuity of care is also important in developing trust and relationship-building."
Understanding the patient
Executives from Franciscan Missionaries of Our Lady Health System in Louisiana; Hospital Sisters Health System's Wisconsin regions; St. Joseph's Health in Paterson, New Jersey; and Trinity
Health Of New England spoke to Catholic Health World about how they collaborate with organ procurement organizations in working with families.
Tanwir Chowdhury, director of nursing for critical care at St. Joseph's Health in Paterson, says St. Joseph's organ donation partner, NJ Sharing Network, has several people who can address families' spiritual or religious questions.
When it is time for a family to make the decision on organ donation, representatives from the NJ Sharing Network meet with them to answer questions. Chowdhury says, "They are well-trained professionals in communication." NJ Sharing Network's
team includes a family service coordinator, clinical donation specialist and hospital service manager to support patients and families through the process.
Network staff stay in touch with the family after the donation to provide emotional support, link them with support groups and connect donor families and donation recipients — when both groups desire that connection.
Anne Pretasky, nurse manager and director of critical care services at HSHS Sacred Heart Hospital, Eau Claire, Wisconsin, and nurse manager of HSHS St. Joseph's Hospital — Chippewa Falls, Wisconsin, says when critically ill or injured
patients arrive at the hospital staff goes into "full treatment mode." Still, there may be opportunities to speak with the patient and family members and learn about the patient's life as staff discuss treatment options and prognosis.
If the time comes to discuss potential organ donation with the family, members of the care team meet with a representative of the hospitals' organ procurement organization to discuss the family dynamics, cultural and religious considerations
and other aspects important to the conversation on organ donation. They anticipate questions and concerns of the family.
Pretasky says that the people authorized to speak directly to the family receive training on the process of requesting donation in a manner that is candid and respectful. To provide emotional and spiritual support to the family in case
the conversation is especially difficult, the hospital usually has a bedside nurse and pastoral care or palliative care staffer in the room along with the individual leading the organ donation discussion.
Be a hero
At Trinity Health's Saint Francis Hospital, representatives with the organ procurement organization — New England Donor Services — have primary responsibility for discussing organ donation with
family members.
"Our goal is to never have a family feel they have been pressured. For us, the most important thing is the interaction as opposed to the 'yes' or the 'no' a family provides," says Steven Averhart, director of family services for New England
Donor Services.
"There is a lot of learning in real-time during these interactions," he says. "Our approaches are not always smooth — grief is powerful and can cloud the understanding, acceptance and judgment of a family member."
Averhart says the objective of the conversation is to guide families to a place where "they can set aside their own grief, if only for a moment, and think about the opportunity of erasing future grief that a stranger in need and his/her
family may experience if they die awaiting a lifesaving gift. More importantly, we want the family walking away with a clear understanding that their loved one can be a hero to someone in need."
Compassion, not coercion, needed for organ donation decisions, ethicist says
Nearly three years after the Centers for Medicare & Medicaid Services finalized a rule intended to increase the supply of donated organs in the United States, some hospitals are seeing unintended consequences for families whose loved
ones are candidates to donate organs.
Under the CMS rule, organ procurement organizations are under scrutiny to increase the number of organs they secure. And in some cases that is leading their representatives to exert a new level of pressure on families who are making decisions
about the potential donation of their loved one's organs. The situation is inviting fresh questions about the ethics around informed consent for donation, the family's role in end-of-life-decision-making and organ procurement organizations'
practices, said John Meinert.

Meinert
Up until recently Meinert was director of ethics for Mercy Fort Smith in Arkansas. He's now an associate professor at Benedictine College in Atchison, Kansas. He presented a July 6 webinar, "Ethical Guidelines for Organ Procurement at the
Bedside."
The webinar was part of the complimentary ethics series, "Emerging Topics in Catholic Health Care Ethics." CHA is presenting the series in collaboration with the Pellegrino Center for Clinical Bioethics at Georgetown University, the Neiswanger
Institute for Bioethics at Loyola University Chicago, and the Albert Gnaegi Center for Health Care Ethics at Saint Louis University.
Act of love
Meinert explained that since organ transplantations began in the U.S. in the 1950s, the Catholic Church has defined organ donation as a gift of self and an act of love, but no person is obligated to give this
gift, nor is a family obligated to designate a loved one as a tissue or organ donor.
Under this ethical line of reasoning, no form of coercion or pressure should be used to obtain permission from a donor or a family member, he said. And, he said, since organ donation is a gift, it is not just informed consent that is called
for — a comprehensive dialogue is needed between organ procurement organization representatives and donors' families, a dialogue that demonstrates that the procurement organization has a holistic view of donors and their families.
This ethical thinking is relevant to the concerns now arising in intensive care units in some U.S. hospitals for patients who are candidates for "donation after cardiac death," the term for patients who are pronounced dead shortly after the
cessation of mechanical ventilation and/or other artificial life supports. It is usual with such patients that their families decide when the mechanical life support is discontinued.
Source of contention
After a family has made the emotionally harrowing decision to withdraw life support, Meinert said, if their loved one is a candidate for organ donation, they then are approached by a representative
of the hospital's organ procurement organization partner. He said that he's seen — or become aware of through research — multiple cases in the last year in which this process has become contentious.
In some of these cases, the organ procurement organization knew the patient declared their willingness to be an organ donor when they got or renewed a driver's license. So, legally, the organ procurement organization had consent to secure
the person's organs, he said. However, in at least one case family members questioned the extent to which that consent also covered the clinical measures that clinicians needed to take to prepare the organs for transplant — measures
that were of no clinical benefit to the patient.
Similarly, in some cases in which patients had not indicated they wished to donate their organs, and their families provided the authorization, the families sometimes regretted that decision because they were not made aware that their loved
one would be kept on life support for several days and be subject to additional invasive procedures including biopsies prior to the donor surgery. The donor's estate or family is not charged for procedures related to organ or tissue donation.
Meinert said in some extreme cases organ procurement organizations have gotten legal teams involved to argue that a patient's driver's license consent to donate an organ also constitutes consent to the clinical steps necessary to prepare that
organ.
Meinert maintained the newly aggressive stance of some organ procurement agencies is directly linked to a revised rule issued by CMS in November 2020. It requires organ procurement organizations to be transparent in their success at getting
and deploying organ donations and compete on their performance. The organizations are then put into tiers, with organizations in the lowest tier being disqualified for recertification.
CMS said the rule change is intended to "support higher donation rates; help shorten transplant waiting lists; reduce discarded but viable organs; and increase safe, timely transplants that save lives."
Meinert said after that agency's ruling, many organ procurement organizations across the U.S. hired new leadership and revised their practices in an effort to increase the number of organ donations they secure. In some cases, that has led
to the problems Meinert described during the webinar.
Need for compassion
He said it is important for the organizations and people involved in organ donation and transplant to view families of prospective organ donors as integral decision-makers. Those who speak to them
about their loved ones' potential donation must be empathetic yet clear about the implications and consequences of authorizing organ donation. Spiritual and chaplain support should be offered to families as they contemplate their decision
under conditions of extraordinary loss and stress.
"These are difficult decisions for families," and those families should be compassionately supported, he said.
Government and organ-sharing organization aim to make organ distribution more equitable
The organization that links the professionals responsible for allocating donated organs among the many people who need them in the U.S. is restructuring the organ prioritization process. A goal is to make that process more equitable.
The Organ Procurement and Transplantation Network has been coordinating the connections needed for organ donation and transplantation in the U.S. since Congress established the network in 1984. A key role of the network is to prioritize
people for receiving donated organs because viable organs are scarce.
Until recently, the network has been using a points-based system that considers each transplant candidate's medical urgency, the federally assigned Designated Service Area the candidate is in, the candidate's biological compatibility with
the donor and the candidate's predicted posttransplant survival prognosis.
Over the last few years, a new fairer system was instituted to remove the arbitrary designated service area border and replace it with a distance within a concentric circle from the donor’s hospital, that is, a concentric circle
of 250 nautical miles or 500 nautical miles depending on the organ. The future policy objective is to remove the bright line concentric circle model to a more sophisticated continuous distribution model.
Additionally, in response to concerns that have arisen about the fairness of the allocation system, a group of private and public organizations has been working to update the prioritization process. This group includes representatives
of the National Academy of Medicine, the Department of Health and Human Services, members of Congress and members of the transplant community, among others, according to information from the Organ Procurement and Transplantation Network.
According to online resources from that network, it has been involved since 2019 in moving to a new organ allocation system called continuous distribution. The new system is expected to be fairer, more flexible and more equitable than
the preexisting system and patients will be able to provide their feedback on the new system more easily.
The continuous distribution system considers multiple factors about transplant candidates at once, rather than placing people into rigid, rank-ordered classifications. While the same types of criteria will be considered in distribution
decisions that were considered in the past, no single factor will dominate decisions on organ allocation under the new system. Factors instead are weighted.
The new system has been put in place for lung, kidney, pancreas, liver and intestine donations and is being put in place for heart donations by 2023.
Watch a video on upcoming changes to the organ distribution system at optn.transplant.hrsa.gov/policies-bylaws/a-closer-look/continuous-distribution/.
— Julie Minda
Saint Francis Hospital offers dedicated room for families mulling organ donation
Saint Francis Hospital of Hartford, Connecticut, has opened a "Donate Life Family Room," which Saint Francis says is the first of its kind in the United States. The room offers a quiet, comforting, private space for family members of potential
organ donors to have discussions surrounding organ and tissue donation, Saint Francis said in a release.
Family members also can gather in the room as their loved one's lifesaving donation is made.
The hospital, part of Trinity Health Of New England, set up the room in partnership with its organ procurement organization partner, New England Donor Services, and with Katie's Foundation, a Connecticut nonprofit named for a woman who
was an organ donor.
The focal point of the Donate Life Family Room is a Donor Memorial tree mural, with each leaf representing a patient at Saint Francis who saved or healed lives with their organ or tissue donation.
As of early August, Saint Francis has had three organ donors this year with 14 organs recovered. Of those 14 recovered, 11 were successfully transplanted into recipients, including a lifesaving heart and double lung transplant. In 2021,
Saint Francis had 13 organ donors. From those 13 donors, 40 organs were recovered and 34 were successfully transplanted. Six organs were used for education and research by the organ procurement organizations.
Copyright © 2022 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3490.