Practitioners strive to preserve the dignity and 'fullness of life' for patients facing chronic illness or death
By JULIE MINDA
The role of palliative care practitioners is to relieve the pain and suffering of people with serious illness and to improve their quality of life. Dr. Ira Byock says there has been a great and pressing need for such care throughout the pandemic.

Dr. Ira Byock
Byock is a leading palliative care physician and founder and chief medical officer of the Institute for Human Caring at Providence St. Joseph Health. That institute aims to promote whole-person care, which it defines as care that is aligned with patients' goals and based in relationships, and that recognizes each patient's physical, emotional, social and spiritual needs.
Byock, who has authored or co-authored five books on palliative and end-of-life care, spoke with Catholic Health World about how palliative care is demonstrating its mettle during the pandemic.
The conversation has been lightly edited for length.
What has the pandemic taught the U.S. about palliative care?
Never in the history of palliative care has the value of this skillset been highlighted as it has during the pandemic. The importance of examining our mortality has become paramount and it's become clear that all of health care occurs against the backdrop of human mortality.
What are the main challenges of providing palliative care in a pandemic?
The main difficulty is that there are not enough palliative care providers to go around. The teams are incredibly strained and stretched, and they are showing obvious signs of wear and tear. A year ago, our palliative care teams were running on fumes and were exhausted emotionally and physically. By late 2020, the fumes were gone, and they were dragging themselves to work, and we were really worried by spring. Then we had a break as vaccination spread and outbreaks went down. Palliative care providers were taking vacations and turning to focus on self-care.
But then the delta surge hit, and we're again legitimately worried about their health and emotional well-being.
Has palliative care staffing been adequate, given demand?
It is important that we acknowledge that the pandemic showed us that there is a shortage of palliative care practitioners, including in Catholic health care. One can hardly exaggerate how stretched our clinical teams are, including our palliative care teams.
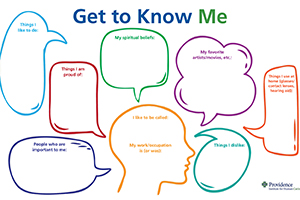
This poster from Providence St. Joseph Health’s Institute for Human Caring can be affixed to a wall in a patient room. It prompts caregivers to get to know their patients as individuals. It’s also available in Spanish.
There has been, in the past, a tolerance for maintaining threadbare palliative care programs. For instance, there are so many palliative care programs that are just available during weekdays or are closed on holidays. Suffering does not take a holiday. Now, with the pandemic, those deficiencies are very hard to ignore.
Within Providence, we've been calling attention to the need to expand palliative care staffing for a long time. Our data showed that there were significant numbers of patients with unmet needs for palliative care. Because of the pandemic, the consequences of not having expanded staffing are more obvious to all.
How are you making the case for increasing the number of palliative care practitioners?
We at the Institute for Human Caring and at our Palliative Practice Group have used this crisis to measure the impact of palliative care. We have shown how it improves the quality of the patient experience and is cost effective in terms of measures like bed use.
Can we improve quality while also diminishing the use of highly burdensome and nonbeneficial care? If so, this is another aspect of a business case for expanding palliative care resources. It's worth looking at the best clinical protocols for situations in which health care resources are severely limited and patients are being given the most aggressive and expensive treatments, without pausing to consider if that is in their best interests — from their perspective.
In American medicine, the prevailing assumption is that more is better. But palliative care practitioners know that often that is not the case. An analytics team at the institute has been showing the real value in aligning what we do in terms of treatment with what people want. The work is also highlighting for senior leadership the important value of palliative care. It's helping us to support the case of expanding palliative care teams. Another advantage of doing this is that expansion can help alleviate the burden on clinicians outside of palliative care teams.
What are some of the roles palliative care practitioners have had during the pandemic?
When it comes to palliative care, it is less about fancy new drug treatments and more about the basics: helping patients understand the treatments for their medical condition, updating them on the physiological aspects of what is happening, and helping the patients and families stay in touch and feel connected.
During the pandemic some of the most poignant roles of palliative care team members have been just holding an iPad so patients and family members can visit, given the visitation restrictions of infection control protocols. They have been part of patient and family meetings. These can be emotional and painful conversations.
It is worth noting that our palliative care teams provide just-in-time resources to guide our non-palliative care colleagues in having conversations about patients' wishes, and we've been providing clinicians with tangible resources to facilitate communication as well as symptom management. It is important for frontline clinicians to have these resources.
In many ministries palliative care teams became involved in policy and protocol development to deal with critical issues such as visitation and the use of medical resources like personal protective equipment and ventilators. This invitation into operational leadership is occurring organically.
What are the main practical challenges to delivering on the promise of whole-person care?
Personal protective equipment has been essential but is obviously a physical barrier to touching patients and to being seen as a person by our patients. We have been sorely aware of the lack of family at the bedside and the difficulties with visitation. Even now, visits are limited to one or two family members. Before the pandemic we encouraged families to visit, bring children, and spend extended time with seriously ill and dying patients. This has been the most difficult strain of this situation.
Families of lower socioeconomic means, who are among those underserved by American health care, have suffered a disproportionate share of COVID-related sickness. I've met multigenerational families living in a single household in which everyone in the home was infected with COVID-19 and the matriarch and patriarch both died.
What have the limits of the pandemic meant for the delivery of palliative care?
It has been very hard to deliver on the full potential of palliative care to ease people's way. The constellation of factors we've discussed — the intensity of the disease and its often-rapid progression, the physical and social barriers required for safety, and our staffing challenges — all inhibited our abilities to provide care to our highest aspirations.
The fullness of human caring involves not just saving and prolonging life, but also doing what patients would value even if a cure is unlikely or impossible. These poignant times offer a chance for them to complete their lives, say things that have been unsaid, express forgiveness and love, and achieve a sense of well-being. People are more than just bodies; we can love, feel loved and experience moments of joy before we die. With our families we can honor and celebrate life and relationships. This is the fullness of life, that palliative care teams strive to preserve.
Now, we can't put lipstick on this pandemic pig. I wish it were otherwise, but many patients are not getting this comprehensive level of care because of the impacts of this pandemic. Palliative care practitioners have had an unflagging commitment to delivering the fullness of human caring and we've tried to do it in an innovative way. In aiming high, even during these difficult times, we have still been able to give really good care.
How are people dying during the pandemic?
Often, not as well as we would wish. We don't have the workforce to always hit the high mark we aim toward. But we've been doing the best we can. We have remained attentive to the dignity of our patients and their pain has been well treated.
Thankfully, we have not had to compromise on the fundamental elements of caring. There's been no shortages of essential medications to alleviate physical suffering. Patients are living and dying in clean, dry beds. We've been finding ways of connecting people within their families and of supporting those families in their emotional suffering and grief.
That is something we can be proud of, that we are continuing to honor their inherent human dignity and worth.
St. Joseph's palliative care team ready for patient surges
This January, the emergency department at Providence St. Joseph Hospital had a peak daily census of 267 COVID-19 patients — more than double the count during a July 2020 caseload spike.
CHA offers resources on palliative care delivery
CHA offers palliative care tools including advocacy information, an advance care planning guide, spiritual care materials, social media infographics, programming development guides and articles at chausa.org/palliative/palliative-care.
Among the resources is "Living Well with Serious Illness," a resource for patients. It is part of a series of publications that CHA created in collaboration with physicians, nurses, theologians and ethicists.
Palliative care teams will find resources including "Honoring the Spiritual Dimension of Palliative Care." It guides palliative care teams through conversations about integrating spiritual care into palliative care delivery.
Dr. Brian Boyd is program director for palliative care medicine at the Orange, California, hospital, medical director for the hospital's home health services and the hospital's chief of staff. He says that while most emergency department clinicians at St. Joseph know that palliative care services are available to help patients articulate their goals of care, they have not always been able to prioritize linking people who are seriously ill with COVID to palliative care team members. This proved especially true amid onslaughts of patients early in the pandemic.
To help ensure COVID patients in the emergency room connect with palliative care providers during what Boyd calls the "golden time" — when they generally are lucid enough to communicate and before they are intubated — St. Joseph late last year established a Goals of Care Center. Boyd says it is especially important to have a palliative care staffer talk to patients and families when there is concern that the invasive intubation could be futile, when patients have low health literacy, or when there is a need to involve family not available at the bedside.

Waite
While that center was decommissioned 11 weeks after it opened because the surge of COVID patients had ended, Boyd says the approach worked well. The palliative care service saw about 125 COVID patients in the ER during that period. Now, a palliative care social worker works five days a week in the ER.
St. Joseph is prepared to reactivate the center if another spike occurs. And the center is serving as a model for other Providence emergency departments preparing for future surges.
Boyd says, "Our palliative care team has been revealed as the best kept secret in the hospital. There has been greater utilization of our team's services (during pandemic-related spikes) with our routine census roughly tripling."
Immediate consult
The Goals of Care Center's palliative care specialists — including doctors, nurse practitioners, nurses and social workers trained in palliative care — maintained an in-person or virtual presence in the emergency department during peak hours.
With the decommissioning of the team, these practitioners have returned to their regular duties at St. Joseph. Boyd says a dedicated palliative care chaplain will be part of the Goals of Care Center should it be pressed back into service.
During their initial run, team members met with the sickest COVID inpatients to discuss treatment options and prognosis so the patients could make informed decisions about invasive interventions and articulate their goals of care.
Palliative care specialists and emergency department staff members together identified patients who would benefit from goals of care consults. When possible, the palliative care specialists would bring into the conversation loved ones whom the patients wanted involved. Due to visitor prohibitions early in the pandemic, many times loved ones had to join the conversation via videoconference. Medical translators were brought in by phone or videoconference.
Boyd says the conversations occurred with both the patients and, separately, their attending physicians and revolved around the realities of the patients' condition, the interventions that might be used and the implications of different interventions. They talked about what the patients' goals were, what interventions were acceptable to the patients, what palliative care measures such as additional pain control were desired and which loved ones should be making decisions if the patients are unable to make them.
The palliative care specialists assisted the patients in documenting decisions, particularly regarding advance directives and followed up with patients, loved ones and clinical team members.
Building the program
Boyd says he and his colleagues had been in conversation with Dr. Ira Byock and other Providence system palliative care experts before the hospital's first COVID surge about how to improve the way palliative care practitioners provide services to emergency department patients at St. Joseph. Byock is founder and chief medical officer of the Institute for Human Caring at Providence.
Prior to 2020, specific clinicians in the emergency department were responsible for ordering palliative care consults. But, under this system, not all patients who could benefit from the consults received them. Also, referrals for consults were not always made at the best time.
Other Providence hospitals have found that embedding a palliative care social worker in the emergency department improves patient access to palliative care.
St. Joseph was preparing in early 2020 to put a social worker with hospice experience in the ER when its first COVID surge began. Given the exigencies, Byock recommended that St. Joseph find a way to further increase its presence in the emergency department.
The Institute for Human Caring aided the St. Joseph palliative care department in creating the Goals of Care Center. The palliative care department initially had the equivalent of one and a half physicians, three nurse practitioners, half the time of one social worker and half the time of a per diem social worker. Leading up to the December 2020 launch of the center, the department added two full-time social workers and two nurses.
The department also began to use videoconferencing to enable palliative care physicians and other specialists from sister Providence sites to provide consults. Boyd said the video connection allowed practitioners to pick up on body language clues that could guide their conversations. The "pop-up" center provided physical or virtual coverage in the St. Joseph emergency department weekdays between 6 p.m. and 10 p.m. In addition, the palliative care staff worked many other hours beyond those times, the hospital said.
Model
Boyd estimates only about 20% of patients who arrive in the emergency department have their advance care wishes documented in the hospital's medical records system. He says that of the COVID-infected patients who come to the emergency department, about half are able to speak and have the mental cogency to have advance planning conversations. Another 25% or so can have such conversations but are challenged to do so because of their condition. The remainder are unable to have the conversation.
Boyd says it's the rare patient who arrives in the ER with a full understanding of the implications of different interventions or of the likelihood of his or her survival.
He says that by having these difficult conversations with patients, and by documenting their wishes, he and his colleagues can ease the burden of decision-making for the families of patients who can no longer make the decisions themselves. Boyd says his team also is lifting a big burden from emergency department staff, as goals of care conversations are time consuming. Without advance directives, clinicians often have to make critical care choices in a vacuum.
Providence is expanding the Goals
of Care team structure to respond to patient surges within its 51-hospital network.
Boyd says when he thinks of the value the center can add for patients, he thinks of Providence's promise: "Know me, care for me, ease my way."
— JULIE MINDA