By JULIE MINDA
About two years ago, a rash of allegations surfaced about egregious mismanagement of veterans'care by Veterans Affairs facilities: military men and women dying as they waited for diagnosis and treatment, administrators manipulating records to hide long patient wait times, veterans growing increasingly frustrated trying to navigate a confusing bureaucracy.
To try to address the concerns, Congress passed the Veterans Access, Choice and Accountability Act of 2014, which in part cleared the way for qualified veterans to access the care they needed from providers outside of the veterans' administration system. Catholic health care providers are among the hundreds of thousands of providers that are offering their services to veterans through the Veterans Choice program.
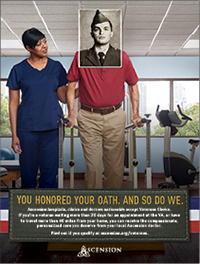
Ascension’s ad campaign lets veterans know that they may qualify to receive care at an Ascension facility through the Veterans Choice program.
"Our participation in this is about reaching out to this vulnerable population — and our message is: ‘There’s help,’" said Nick Ragone, chief marketing and communications officer for St. Louis' Ascension. All Ascension providers began offering veterans services through the Veterans Choice program early this year through a national contract between the 137-hospital system and two third-party administrators that are the contractors for the program.
Matthew Grimshaw, president of CHI St. Alexius Health in Williston, N.D., another Veterans Choice provider, said he hopes the program leads to "improved quality of life for veterans, so that we treat them in the community instead of making them be treated differently than everyone else."
Time and distance
According to Kristin Cunningham, director of business policy for the VA office for community care, Veterans Choice aims to "ensure vets get the best care in the environment that works best for them."
Through the program, health care providers contract with third party administrators TriWest Healthcare Alliance or Health Net Federal Services — each is responsible for certain geographical regions in the U.S. — to join the Veterans Choice network. Providers must agree to accept Medicare rates, have the same or similar credentials to VA staff and agree to submit medical records for the care they provide to the VA for its electronic medical record system, among other qualifications. According to Joseph Duran, acting director of community care operations for the VA, about 260,000 providers had contracted to join the network as of Feb. 1.
For a veteran to use the Veterans Choice program, at least one of the following situations must apply:
• Live more than 40 miles driving distance from the closest VA facility.
• Have to travel by plane or boat to their closest facility.
• Be unable to get an appointment for care at a VA facility within 30 days of the date the veteran’s usual VA provider says that person needs to be seen.
• Have an unusual burden traveling to the closest VA facility to receive care.
• Have specific health needs that warrant special consideration, as determined by VA staff.
• Live in a state or U.S. territory without a full-service VA medical facility providing certain services.
Single point of entry
Veterans call a toll-free number to be screened for eligibility and then, if they qualify, to enter the program. They supply information so their eligibility can be determined, choose their preferred health care provider and report whether they have other health insurance. If they are eligible for the program, and if their preferred provider is part of Veterans Choice, they then schedule their appointment on that same phone line.

Grimshaw

Ragone
All appointments must be arranged through the toll-free number, which is manned by the third-party administrators, and all care must be preauthorized by the VA before the provider can deliver it.
The VA pays all costs for treatment of service-related injuries. Veterans who have other health insurance, such as private insurance from a civilian employer, will need to pay applicable co-payments or deductibles. That other insurer will be billed for non-service related conditions.
The legislation that established Veterans Choice allotted $10 billion. Veterans Choice will expire when the funds are depleted or by Aug. 7, 2017.
Navigating Veterans Choice
Ragone said Ascension contracted as a system to join the Veterans Choice network because contracting nationally is in line with the system’s "One Ascension" approach of functioning as an integrated system. About 2,000 Ascension sites across 24 states and in Washington, D.C., are part of the contract. All of Ascension’s employed physicians are taking part. The system is encouraging its affiliated physicians who are not directly employed by Ascension to do the same.
Ascension has hired dozens of veterans to staff a call center and to serve as navigators for military men and women accessing care at Ascension sites. Ragone explained, "These roles are staffed by veterans because we’re very aware that veterans have very special needs. These navigators understand those specific needs and how to work with vets." He said the navigators and call center staff will help the patients as they are working with the VA, the third-party administrators and the providers.
Recent news reports have said that veterans are experiencing difficulties accessing Veterans Choice, including long wait times and confusing bureaucracies. Ragone said the Ascension call center and navigators should ease such concerns for patients accessing care through Ascension.
Ragone said in preparing to serve military men and women through this program, Ascension understood that veterans are different than the general patient population. Veterans may be at risk for post-traumatic stress disorder, suicide and other mental health concerns; and their combat-related physical injuries can be very different from those of civilian patients. Ascension offered its providers in-person and online training on the special needs of veterans, and it has established a website, ascension.org/veterans, where providers can access additional information and training. Ragone said providers "are fully prepared to listen and understand the physical and emotional needs of these patients and to ensure they receive the right care."
Ascension has launched a media campaign throughout its service area that includes social media, print and broadcast marketing to alert veterans to the care option.
Ragone said, "I’ve never before seen our 160,000 associates so energized by a program. We’ve received scores of emails from associates who are so proud to be a part of this. It fits so beautifully with our mission."
Four hundred-mile drive
Grimshaw said CHI St. Alexius, which is in northeastern North Dakota, was working with elected officials even prior to the scandals to advocate that veterans receive care in their communities. The Williston area is more than 400 miles away from the nearest VA specialty facility. Veterans had to drive for hours and often incur hotel costs to get care. Those with jobs had to take off a day or more of work.
Grimshaw said at roundtables a North Dakota senator held several years ago, veterans shared their frustrations with this situation, and civilians in the audience "couldn’t comprehend how these veterans had to drive for hours for every medical service they needed," beyond primary care provided at a local VA clinic.
Grimshaw said CHI St. Alexius clinicians have treated dozens of veterans through the program since the hospital joined Veterans Choice in July 2015. He said he and his staff appreciate the ability to care for military men and women. "We’re taking down the barriers that separate care of the veteran from the care everyone else receives," he said.
Ascension’s Ragone added, "Hopefully, we will be able to get more veterans into the system (through Veterans Choice), instead of them being on the outside."
| Veterans Affairs department addresses access issues
A Government Accountability Office report has found concerns persist for veterans trying to access health care through the Veterans Affairs department's Veterans Health Administration, despite reforms put in place after the 2014 scandals related to patient waiting lists and appointment scheduling.
An April 19 GAO study found that about one-third of veterans newly enrolled in VA benefits and requesting to be seen by a VA provider had not been seen promptly by providers, nearly half were unable to access primary care due to scheduling problems, and poor VA scheduling practices were contributing to unnecessary delays. Just prior to that report release, on April 8, Dr. David J. Shulkin, undersecretary for health for the VA had announced "MyVA Access," a new VA initiative to improve care access. Aimed at providing more "veteran-centered" care, the effort will offer same-day appointments at VA facilities when such prompt care is medically necessary; a smartphone app that will allow veterans to schedule and track their appointments; and a website feature that will allow veterans to check wait times in real time. These features now are available on a limited basis. The VA plans to make them available at all of its medical centers in the future. |
Copyright © 2016 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.