By KATHLEEN NELSON
Before earning her nursing degree, Deanna Selk worked as a technician in the intensive care unit at Mercy Hospital Oklahoma City. She knew that after graduation, she wanted to work at the hospital as an ICU nurse. Even though she seemed to have a clear idea of her career path and some knowledge of the unit, she wouldn't have felt as ready for her first day of work without the hospital's new program for recent graduates, the Nurse-Resident Learning Center.
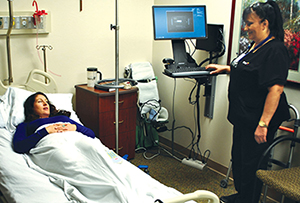
Indira Rai-Choudery, standing, hones her communication skills and electronic medical record documentation know-how with a practice assessment of Mary Lawrence at the Nurse-Resident Learning Center at Mercy Hospital Oklahoma City. They completed their new nurses training in July 2015.
"This program helped me bridge the gap from nursing school to RN by providing me with focused education," Selk said.
For a new nurse, the transition from school to hospital can prove intimidating, even frustrating. A study from the RN Work Project found that the one-year turnover rate among newly licensed RNs was 17.9 percent; the two-year rate was 33.5 percent. Mercy's goal for the program is to keep its recent hires by giving them the tools they need to make the transition and begin their careers with confidence.
Listening to nurses
Karyl James, chief nursing officer at Mercy Oklahoma City, said the program grew out of feedback from new nurses over several years. In the past, Mercy had assigned a new grad directly to a unit, where he or she learned the ropes from a preceptor, a nurse mentor.
"We were asking a nurse with a full load of patients to also teach how to be a nurse. Depending on the workload for the day, the instruction was variable because the process was inconsistent," James said. "The new nurses said they needed better up-front training. They were uncomfortable, they were scared and had a lot of anxiety taking on that patient load for the first time."
James led a group that designed a training program to provide more consistency in training and give new nurses more opportunities to develop skills before working on the floor.
Hiring for fit
Rather than hire a graduate to work in a specific unit — ICU or oncology, for example — all new nursing school graduates hired at Mercy Oklahoma City are assigned to the learning center for eight weeks of training.
"All are hired for fit to work at Mercy," James said. "They have background, drive, they want to be a nurse and they have a sense of mission. Some graduates don't know where they want to be. Some have a clear idea. We help facilitate that career path."
The new nurses are trained in a dedicated space that includes separate computer and simulation labs, and they sample different specialties. Some sessions are taught by the learning center staff, others by nurses in the specialty. On Monday, for example, they might have lectures on cardiac assessment. On Tuesday, they practice it in the simulation labs. On Wednesday, they regroup to discuss further what they've learned. The nurse residents also spend time each week in the computer lab, learning to use the electronic record system.
Building confidence
"We all learned the hospital-wide core competencies from the same person," said Lynn Ann Feroli, who went through the nurse residency program and is working in the neonatal ICU. "There won't be a question of what and how it was taught because the same person is doing it all. Also, doing these core competencies in a neutral environment takes away the stresses caused by being a new nurse on the floor. You can focus just on those specific core competencies and not have the added stress of department-specific expectations."
The program also includes shadow days, which give nurse residents a chance to work with several disciplines. Selk worked with physical therapy, the wound/skin team, the pain team, stroke team and the diabetes educator.
"Some of our newer nurses have said, 'I never wanted to be in oncology but now that I've tried it, I don't want to be anywhere else,'" James said. "I think it's a surprise for them."
Following the orientation and training program, nurses are assigned to four weeks in a specific unit, based on their interests. Selk was assigned to ICU, even though "I did come to realize that I also liked working in the step-down unit and the ED. Before, I never considered any other option other than ICU, but now I know I would like to be cross-trained in either of those departments."
Selk's training in the ICU progressed smoothly. "On my first day with my preceptor ... she said it was great that she didn't have to focus on training me how to chart or how to use the equipment, but that she could focus on being an ICU nurse."
The first graduates of the program entered their units in September, and a second group was permanently assigned in December. James said that eventually she hopes to start a group of as many as 10 new graduates every four weeks.
"By the time they get to the floor, our preceptors are telling us the new nurses are taking patients on their own from the first day," James said. "I've never seen that before in my nursing career. I know I wouldn't have felt comfortable doing that. They are confident. They know how to document in the electronic records. They know how to get medications."
Selk said: "The learning opportunity I received at Mercy as a new nurse is one I don't think I would have received anywhere else. I'm extremely proud that I work for a hospital that is committed to the success of new nurses."
Copyright © 2016 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.