Hawaii is first in the nation by many measures of health and well-being. It tops the Gallup-Healthways' Well-Being Index, which gives it bragging rights as the happiest state
By JUDITH VANDEWATER
HONOLULU — Hawaii is first in the nation by many measures of health and well-being. It tops the Gallup-Healthways' Well-Being Index, which gives it bragging rights as the happiest state. With an average life expectancy of 81.48 years, residents live 2.87 years longer, and with less disability, than the U.S. average, according to the U.S. Census Bureau.
But Hawaii also has the nation's highest cost of living, and this distinction, combined with longer life spans means the state and its families are sure to face a heavy economic burden caring for the very old, particularly people with Alzheimer's disease and other aging-related dementia.
Demographers predict that in Hawaii, as in the U.S. as a whole, the percentage of people 85 years or older will grow the fastest of any age group in the next few decades. The Census Bureau estimates that 8.7 million people in the U.S. will be age 85 or older in the year 2030. Studies have shown the incidence of dementia, particularly Alzheimer's disease, increases significantly with age.
It was against this backdrop that The St. Francis International Center for Healthcare Ethics hosted "Caring for Our Ku–puna: Balancing Human Dignity and Economics." (Ku–puna is the Hawaiian word for elder or grandparents.) The daylong conference drew about 270 participants including economists, lawyers, ethicists, geriatricians, palliative care and hospice clinicians, and professionals who provide social services for the aged. They heard speakers and panelists explore thorny questions to which there are no clear answers. The questions include how society should mitigate the competition for financial resources between the young and old, and between the relatively small number of very sick, very expensive patients and the health care needs of everyone else.
The St. Francis ethics center is part of St. Francis Healthcare System. The system got out of hospital care a few years ago, but it remains one of the state's largest providers of health services. Its core health-related businesses, which include hospice and palliative care, home health, home bathing services, principally serve elderly patients.
As part of the ongoing reset of its ministry, St. Francis also is addressing Oahu's scarcity of affordable senior housing and its shortage of nursing home beds. In 2011, it completed Franciscan Vistas Ewa. The 149-unit apartment complex in Ewa Beach is open exclusively to low- to moderate-income seniors. It has a 600-person waiting list for tenancy. Next year, St. Francis plans to reopen three floors of its shuttered hospital in Honolulu's Liliha neighborhood as a 100-bed skilled nursing facility. It hopes to build affordable independent living apartments and offer assisted living on the campus in phase two of that development.
Care of the vulnerable
The bioethics conference was Aug. 9, the anniversary of the death of St. Marianne Cope, foundress of the St. Francis Healthcare System. A Catholic nun from Syracuse, N.Y., St. Marianne came to Hawaii in 1883 to care for people with leprosy on an isolation colony on the island of Molokai. Dr. Faith Fitzgerald delivered the St. Marianne Lectureship at the conference, drawing an analogy between the outsider status of today's "demented, frail old" and the isolation and suffering endured by people with leprosy back when the disfiguring disease had no effective treatment.
Fitzgerald, a professor of internal medicine at the University of California, posited that, as a species, humans may be hardwired not to empathize with (non-related) people who don't physically resemble them, including individuals whose advanced age has changed their appearance and functional abilities. She said in human evolution, advanced old age is a modern-day development. "Maybe the ability to identify old people as human beings never fully developed in the ancient brain because there were so few old then," Fitzgerald said.
Timothy T. Taylor, an economics lecturer for The Teaching Company and the founding editor of The Journal of Economic Perspectives, mapped out some of the financial challenges ahead in caring for the growing population of people who will reach advanced old age, many after decades of progressive disability and increasing dependence on caregivers.
About two-thirds of people 85 and older have "functional limitations," and most receive assistance in daily life from family members and friends, according to the Congressional Budget Office. The National Institutes of Health-funded Health and Retirement Study indicates that more than 18 percent of people aged 80 to 89, and almost 30 percent of people aged 90 and older have Alzheimer's disease. Taylor said that, per capita, Alzheimer's patients have the highest care costs in the U.S. health system.
The CBO estimates that, in 2011, 55 percent of the care provided for elderly people in the United States was uncompensated care provided by family or close friends. Taylor told the conference that it will become increasingly difficult to find the volunteers to care for frail seniors in their homes in coming decades as primary caregivers age along with the growing numbers of those who will need assistance in tasks of daily living. Nevertheless, it will be important to the country's overall economic health to provide services that allow people to remain in their homes and out of residential care facilities for as long as possible. In part this can be achieved by designing communities and homes to be more accessible and age-friendly, he said.
Do no harm
Participants in a panel discussion on end-of-life care laid out some of the pressures that come to the fore when there is disagreement among family members over what medical treatments are appropriate for a patient who is at the end of life. Such disagreements arise even when a patient has an advanced directive, the panelists said. Fitzgerald, who moderated the panel, said that in her internal medicine practice she has found that the family member who is the most estranged from the patient is the most likely to argue for prolongation of life, at any cost, even when the intervention would prolong the dying process.
Dr. Carolin Hubbard of Honolulu, a specialist in hospice and palliative care medicine, said often an adult child living on the mainland or in another country has the hardest time accepting a parent's impending death and may resist a doctor's recommendation that the patient receive only comfort care. "We started using Skype," she said, referring to the program that transmits live video and voice over the Internet. "Having them see the individual sometimes helps the person who is at a distance to understand what is happening and feel included," she said.
Dr. Anna Loengard, chief medical officer for the St. Francis Healthcare System, said that treatment decisions should be based on "what is appropriate medical care." Loengard, a gerontologist and specialist in palliative medicine, said that in Europe doctors would not consider complying with a family's demands for care that is not medically appropriate and could increase a patient's suffering. She said that she encourages her patients to talk with their family members and caregivers to clarify the desires underlying the patients' advance directive. "You are never going to be able to write down what you want for every medical situation; it is better if they know your intent," she said.
In the footsteps of two health care saints, St. Francis seeks out underserved
Editor's note: CHA President and Chief Executive Officer Sr. Carol Keehan, DC, toured the site of the leprosy colony at Kalaupapa, on the Hawaiian Island of Molokai in advance of The St. Francis International Center for Healthcare Ethics bioethics conference. Now a National Historic Park, Kalaupapa was an isolation colony where thousands of victims of Hansen's disease lived and died in forced exile. In the 1940s, sulfone antibiotics proved effective against the disease, but it was not until 1969 that Hawaii abolished its 100-year-old isolation law. A small number of patients still live in the community, although they have not been bound there for decades.
 By SR. CAROL KEEHAN, DC
By SR. CAROL KEEHAN, DC
CHA president and chief executive officer
Molokai reflects the immense beauty Hawaii is noted for. Yet its name evokes a sense of incredible suffering and gross disfigurement. The more one reads about the history of Molokai, the more it lives up to its reputation.
The criminalization of sickness led to thousands being taken from their families and shipped on a cattle boat to grossly inhumane conditions on a remote island. Lack of food, shelter, safety and health care were the norm and even the ability to be buried with dignity was absent.
The church has recently canonized two very different people who felt compelled to respond to this appalling treatment of God's children. St. Damien de Veuster and St. Marianne Cope brought very different personalities, styles and gifts to the care and support of patients with leprosy (Hansen's disease). Their extraordinary efforts to improve the lives and care of patients have inspired generations. The opportunity to walk in the footsteps of these great saints and appreciate the suffering they were responding to is a great grace and inspires us in health care facing challenges in obtaining appropriate care and services for people undervalued by much of society.
St. Marianne's Franciscan sisters and St. Francis Healthcare System continue to seek out those underserved and to share the story of St. Damien and
St. Marianne to inspire us in our efforts to do the same today.
Conference speaker says filial piety is the law in Singapore
By JUDITH VANDEWATER
Honolulu — The Chinese character for filial piety is represented by an elder sitting on the shoulders of a descendent. In Singapore, it might also be appropriate to perch the descendent atop a law book. That's because the island nation's Maintenance of Parents Act makes it compulsory for adult children to contribute to the support of an indigent parent. The state, which does not offer social security insurance, is the safety net of last resort.
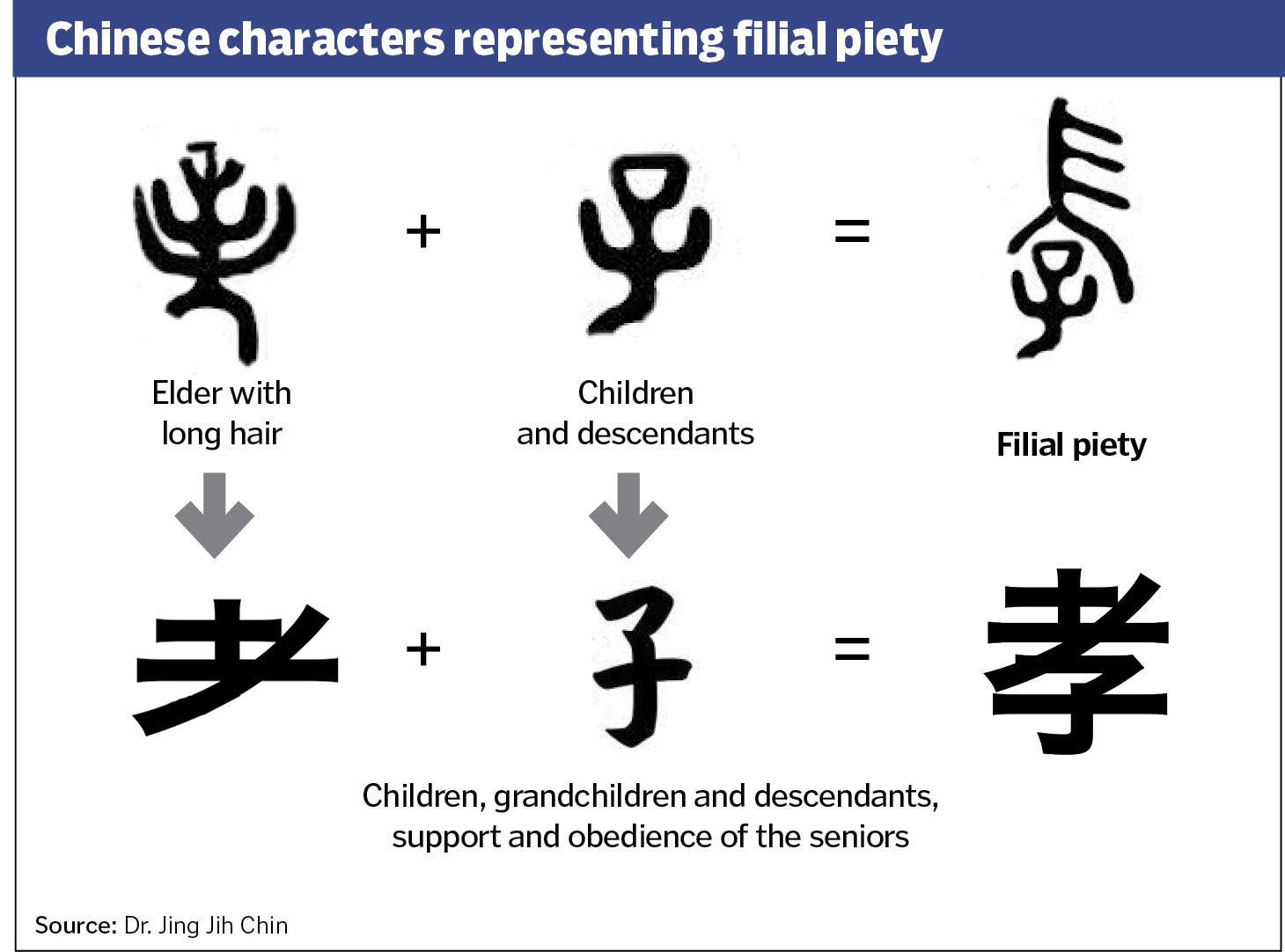
Filial piety is a key virtue in the Chinese culture, and ethnic Chinese make up most of the population of Singapore, Dr. Jing Jih Chin told the audience at the international bioethics symposium here. The dominant religions in Singapore — Buddhism, Christianity, Islam, Hinduism and Confucianism — convey a moral obligation to honor and care for one's parents, he said.
But economic and time pressures of modern family life have taken a toll on filial piety, and Chin said a concern that an increasing number of parents were being financially abandoned by their adult children led to the passage of the unusual legislation in 1995. Walter Woon, the former Singapore parliament member who wrote the law, intended it to kick in when filial piety fails. "The law cannot legislate love between parents and children and husbands and wives," Woon wrote in a 1994 Wall Street Journal article. "All the law can do is provide a safety net where morality proves insufficient."
Chin said all children — irrespective of their birth order, and whether they are natural progeny or adopted, or were born inside or outside of a legal marriage, or have a good or poor relationship with the indigent parent — have a potential financial obligation under the law.
When an elder brings a financial claim under the law, the parties must participate in a counseling/conciliation process. If that fails to bring an agreement on the amount each child will pay, the case is brought before a tribunal, Chin said. The legal proceedings and files are closed to the public. "There is no public shame … people aren't named in the papers," he said. "The whole thing resonates with the public's view of fairness," said Chin, who is an ethicist, geriatrician and president of the Singapore Medical Association.
Copyright © 2013 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby
or call (314) 253-3477.